Safe Sleep For Infants: SIDS & SUIDs
The slogan “Back to Sleep” which revolutionized infant sleep methods has been changed to “Safe To Sleep” to broaden its scope and bring other causes of sleep-related infant death “into the fold” for research. Perhaps you already knew that, the slogan has been registered as a trademark of the US Department of Health and Human Services.
“Back to Sleep” slogan now “Safe to Sleep”
However, “a name is a name is a name is a name” – unless it’s meaningful in preventing infant deaths.
Back to Sleep, Safe Sleep, SIDS, SUIDs
Just slogans and names unless we can prevent deaths
The “back to sleep” campaign was highly successful. In just a short time nearly all parents got the point and clearly understood the issues. Lets hope that “safe to sleep” does as well. We certainly need parents to stay focused on all the other issues we’ve found in order to keep the overall infant death rate on the decline.
Sleep-Related Deaths in Infancy

And keeping up with the latest safety recommendations like you do, I’m sure you are aware that, just in the United States alone, more than 4,000 sleep-related sudden infant deaths (SUIDs) occur every year.
Politicos just can’t leave the single most widely-known, clearly-defined medical issue, SIDS (Sudden Infant Death Syndrome), alone.
For whatever political reason that fancied them, not only the slogan has changed but the classification too – to include back into the “research umbrella” those deaths that had been removed from the SIDS classification because we now understand are attributed to things like suffocation, asphyxia and strangulation.
One common denominator in all of these is the sleep environment. In Florida researchers found that 80% of all sleep-related SUIDs occurred in infants placed in unsafe sleeping environments. Eighty percent! In my book that’s almost all of them.
SIDS

You see we have NO biomarkers for SIDS! That means we have absolutely NO WAY of telling that a baby died of SIDS by testing or physical exam. What we DO do is to examine and research every case for ALL KNOWN CAUSES and when all of them turn up negative we assign the cause of death to “SIDS.” When we’ve done all that, it still makes SIDS the leading cause of death for infants 1 to 12 months of age!
As more and more research has occurred we find “other cause” after “other cause” and take them out of the total figure – that makes the number of SIDS deaths statistically go lower and lower. BUT, that doesn’t mean we’ve ‘cured’ that group of kids – unless we also find a remedy we can pass on to parents.
Such was the case, you remember, when we discovered that some infants were dying of botulism toxin from the spores in the honey they were being fed. Spores that don’t effect an adults intestinal track but do effect the immature infant’s.
The number of SIDS deaths decreased (because we now knew the cause) but the actual number of infant deaths didn’t decline until enough parents got educated to stop giving infants honey.
Researchers in the field now call it the “triple hit theory.” SIDS occurs in: Strike one – a vulnerable infant; Strike two – during a critical period of development (<6 months greatest risk); and, Strike three – exposed to a “risk factor” such as prone position, over bundling or airway obstruction.
Protection From SIDS

Here’s the deal: we really shouldn’t be touting “protection” from SIDS; because, we really aren’t certain of anything that “protects” against SIDS. Nothing is certain. We only have hundreds of statistics, none of them are certain and some are conflicting.
If you want me to list some of the possibilities I will. For example, when we look at SIDS statistics we notice that there seems to be less SIDS when the baby is breastfed. That DOES NOT MEAN, in any shape or form, that we’ve discovered breast feeding “prevents” SIDS! There is no evidence that it does. We simply are reporting that there seems to be less of one if the other is true.
However, we do see some “dose related” effects in the statistics; meaning, the “drop in SIDS incidence” seems to be related to the “dose” of breastfeeding. One study showed a “45% reduction” for partial or short-term breastfeeding to “73% for exclusive breastfeeding”; which is quite unrealistic. Oh, nobody is contesting the math – numbers are numbers – but just logically, 25% more percent and and there would be “Zero” SIDS, which is just not seen at all in “real life.”
Additionally, whether breastfeeding can counteract other modifiable or non-modifiable risk factors like smoking, co-sleeping etc. is still completely unknown; which, could mean that other completely different rationale are at play here and not just the breastfeeding.
Is it good to breast feed if at all possible – most certainly YES. Does breastfeeding “prevent” SIDS – it would be nice if it did; we can hope; some people think there may be a link; we’d be foolish not to try it if we can.
However, please don’t get the idea that breastfeeding is the “cure” and you don’t need to worry about the other “risk factors” which have some statistical relationship to SIDS: smoking (both prenatally and postnatally), co-sleeping and drug and alcohol use (especially combined with co-sleeping).
Additionally, keeping both the infant’s and family members vaccinations up to date is critical – of course, combined with vigilance against exposure to any known sick persons.
“Safe to Sleep” and Sleep Position

Supine sleeping (on your back) was the first major change in the campaign to prevent SIDS and is still the cornerstone of “Safe Sleep” because we actually have data that it has lowered the number of total infant deaths.
But, “Safe Sleep” is more than mere “Back Sleep” because we now recognize that nearly everything about the environment is important to protect the infant – bedding, clothing and temperature of the surrounding air have some data to suggest their correlation to SIDS.
Supine sleep should begin at birth and continue until the infant can roll from supine to prone and back again. AND, it should be used for EVERY sleep including naps AND in every setting including daycare, relatives homes, busses, cars, trains, airplanes… you get the picture. Once they can roll over both directions they can remain in the sleep position they assume.
Prone sleeping is not the only risk, many infants who died were found prone after being placed on their sides to sleep with positioning devices; therefore, never use wedges, rolled-blankets or positioners and exclusively use the supine position.
Risk of Choking Myth
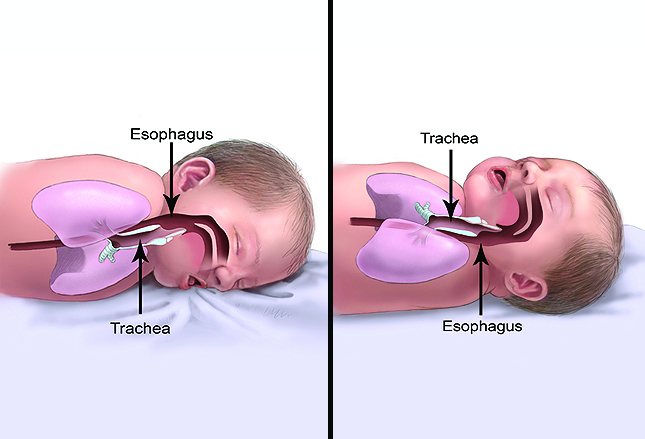
It’s natural to assume that because we usually put infants down to sleep after feeding, and because they “wet burp” a whole lot, there would be an increased risk for choking if they did it while lying on their back; but this is NOT the case.
The diagram shows that the esophagus (the route stuff will come from the stomach) is ABOVE the trachea (the route into the lungs) when lying prone. That means any “burped” stomach contents will, by gravity, land on the open epiglottis and flow into the lungs.
Lying on the back, the esophagus is BELOW the trachea so gravity naturally takes liquids out and away from the lungs.
The SAFE Crib

An infant sleeping supine on a firm mattress and tightly fitted crib sheet is in the safest sleep position we know about. The SAFE crib contains nothing but a supine baby!
There are no bumper pads, quilts, blankets, pillows, toys, positioning devices or reachable toys with strings in a SAFE crib. Nothing. Latest safety standards describe slat construction and spacing as well as disallowing drop-down sides which were associated with injuries and deaths from entrapment.
Pre-2011 built cribs are not considered safe any more.
Everyone knows to avoid soft bedding that could cover a baby’s face; but, it is equally important not to place soft bedding UNDER a baby. You may erroneously believe such softness gives them added comfort but it does not – it only increases risk of CO2 retention around the baby’s mouth and nose which slows respirations as well as obstruction to the flow of oxygen. ONLY use a tight fitted bottom sheet which cannot come loose.
The UN-safe Crib

Just to drive home the point and counter all the crap advertising you’re bombarded with, this photo is of an UNSAFE crib. A study showed that 66% of parenting magazine images depicted UNSAFE sleeping environments.
Do not in any way think that these practices are “normal” let alone desirable. Yes, the use of hazardous bedding has declined but it is still highly prevalent among younger, nonwhite and non-college-educated mothers. It seems that just because someone recognizes the danger of soft bedding on top of an infant it doesn’t mean they heed warnings about soft bedding beneath the baby.
True to form – the scammers loosing their sales and profits invented their own “solution” and began selling what they CLAIM are “breathable mesh liners” and touting that they “prevent suffocation.” These claims are blatantly false and, in my opinion, should be a jail-able offense. Such liners are not only unnecessary but ARE potentially dangerous and have absolutely NO role in “reducing suffocation.”
Room Sharing

I have to admit that this one still “grates” on my nerves a bit; but, there does seem to be some data that sleeping in the parents bedroom is a bit “safer” for infants through the first 6 or so months. I just wish I could believe it!
What the studies DID NOT even address is all the other issues we’ve tried to solve by recommending the baby has it’s own room – sleep deprivation, frequent awakenings (both baby and parents), inappropriate nighttime behavior training from sheer desire to get back to sleep, etc. etc..
The statistics are similar to the ones about breastfeeding mentioned above; namely, there is NO real “smoking gun” but only numbers that “seem to show.” And we don’t even really know why there may be safety but we conjecture that, at least in some families, there may be closer monitoring of risks for suffocation, strangulation, entrapment or the like.
There is a closer proximity for feeding regardless of method; but there then becomes the temptation to fall asleep while breastfeeding or place the infant in the parents bed – both bad ideas.
NO Bed Sharing

Pure and simple, more than HALF of all recent sudden and unexpected deaths in infants occurred in a bed-sharing situation, meaning that an adult or child was sleeping on the same surface with the baby.
At least 45% of parents in the US admit to bed-sharing and it’s even more culturally entrenched in other parts of the world but is a factor in high numbers of sudden infant deaths. Reviewing 102 infant deaths in Maryland, 45% were found to have been co-sleeping.
The risk of co-sleeping is even greater if parents smoke, drink or use drugs – including some prescription drugs.
Free crib programs exist for low-income or high-risk families and should be sought out by contacting health-departments, local hospitals or physicians offices.
Blankets and Sleep Clothes

There are no research data available about SIDS and sleep clothes – as long as they in no way can cover the infants face or are inappropriate for climate or size. The recommendation for a one-piece sleeper or sleep sack comes as much from other parents as it does from us docs.
Trying to work with the mandate for “nothing in the bed but the baby,” a “onesie” just seems to fit the bill. No swaddling or blankets are needed and the weight of the material should be appropriate for the season.
IF a blanket must be used the infant should be placed with its feet at the foot of the bed which lessens the risk of the head becoming covered. The thin blanket is then tucked in on three sides with the top not higher that the baby’s armpits – i.e. nowhere near the face.
An infant sleep-bag should be the correct size and have fitted neck and armholes or sleeves for warmth BUT no hood. That way there’s not even the slightest chance the head might become covered.
And just so you’ll know, there is no evidence to date that supports the added expense of sleeping sacks or bags preventing SIDS despite internet claims.
Where NOT To Sleep

As easy as it is to let slip by, sleeping on a sofa or in a chair with an infant should always be avoided because of the significantly increased risk for SIDS. Thirteen percent of sleep-related infant deaths occurred while co-sleeping on a sofa!
Especially in the first months before they learn to sleep through the night, parents must not put themselves in a position where they even MIGHT fall asleep so-sleeping with the baby.
Sleeping upright is dangerous for a newborn due to their relatively heavy head and weak neck muscles. The head can loll and drop and easily block the airway. That makes sleeping in car seats, strollers, swings, baby carriers and slings equally dangerous. They should never be propped in a sitting position to sleep.
Cloth baby carriers easily allow babies to slide down and drop so the face is buried in the fabric. Any time a baby carrier is used parents should make certain the infant’s face is always visible and above the fabric with the nose and mouth unobstructed.
Pacifiers and Sleep

Another oddity of statistics shows that the use of a pacifier for naps and bedtime is protective against SIDS – even if it falls out of the infant’s mouth! Go figure. In other words, parents do NOT need to keep replacing the pacifier during sleep.
DO NOT introduce a pacifier before 3 or 4 weeks of age but it may be continued up to year of age while the need for sucking is strongest. After that there is no logical rationale for using one and the dentists then begin making demands toward mouth, gum and tooth health which prohibit the devices.
Never hand a pacifier around an infants neck due to the risk of strangulation. And DON’T use the type which attach to the clothing on a sleeping infant – sorry guys, it’s good to know you don’t have to keep replacing it though isn’t it?
Warmer Is Not Better

The reason that Christmas movie showing the kid bundled up into a round ball of clothing was so funny is because… it’s true. Many parents do have a tendency to overdress infants, and even cover their faces, when out of doors.
Like other things we’ve mentioned here, the thermal stress from overdressing or overbundling is just like exposure to high temperatures and is associated with higher risk for SIDS.
To dress an infant appropriately for the environment they should have no more than one more layer than an adult would wear to be comfortable; and the air temperature should be adjusted to the comfort level of an adult
Continually evaluate the infant for signs of overheating keeping in mind that children don’t have the ability to sweat like adults. If you notice moisture on an infant’s skin (usually chest) it means they are a lot hotter than you think. Breathing faster, being irritable, and flushed skin can be signs of overheating.
You never want to bundle over an infant’s face and if fans are used to obtain some air movement you don’t want it blowing directly on their face. That triggers an automatic reflex which causes them to catch their breath.
Tummy For Play Not Sleep

Now for the fun part of this whole article – tummy time is for play and it should begin the day you bring the little one home from the hospital. All this back sleeping can actually “flatten” the back of a baby’s head as it’s firming up and growing together. That actually was a sign we were taught to look for which was commonly seen in orphanages where babys were rarely picked up.
The point of beginning tummy time early is to strengthen head and neck muscles. However, for infants, tummy time is like going to a public swimming pool – there needs to be a “lifeguard.”
Supervised daily “tummy time” is best if used as a “bonding” time with mom and dad, when begun early, when accomplished regularly, with energy and with joy. You can use toys or even your own face to encourage them to lift their head.
You can do it on your chest or a flat surface. You can do it two or three times a day beginning with short 3-5 minute sessions and extend durations as they enjoy the experience. You’ll start to see improvement in muscle tone faster then you think.
Word Is Not Out Yet
As a parting shot I should tell you that after the Back To Sleep efforts began we started to see a steady decline in SIDS. It was really working. Each year the incidence dropped even more.
After years of improvement the SIDS rates have plateaued. Are we done? Does everybody who should know, know? Are there still hold-outs who haven’t been reached or convinced? Can we lower the SIDS rate even lower – or is that all there is?
Advertisement by Google
(sorry, only few pages have ads)

