Common Pediatric Recreation and Sport’s Injuries – Part Two
Thirty-six million kids participating in organized sports across the US means that 2.6 million of them will be treated in ERs this year with sport’s injuries – and that’s not counting informal recreational activities or kids over 19.
One in twelve child sports participants visit the ER
Our discussion of children’s fractures took up an entire post which leaves basically all the “non-fracture” stuff, if we want to keep listing the most common injuries that physicians see resulting from sports and recreation.
Recreational and Sport’s Injuries in Kids
What’s left to talk about after removing everything related to bones? Well there’s still sprains and strains – which are about muscles and tendons. And there’s heat-related illnesses, concussions, cardiopulmonary, infections and exposure to insect species. Let’s get crackin’!
Sprains, Strains and Ligaments Oh My
The most common childhood sport’s injuries are sprains and strains and ankle sprains lead the pack in “common-ness.” Eighty-five percent of ankle injuries are due to inversion which damages the lateral ligaments and is due to running on uneven surfaces.
In elementary and middle-school aged children, growth plate injuries are more common than ligament injuries so smart doctors seeing children always check for them whenever they see the other.
Doctor’s have developed sets of algorithms to help decide whether or not X-rays will be useful in adolescent injuries and you’ll commonly see us get X-rays of BOTH SIDES even though only one is injured. That’s because we often can’t make the correct diagnosis in growing teens unless we’ve got a “normal” limb to compare it with.
We do the same thing with our physical exam; namely, comparing the “good limb” with the painful one for bruising, tenderness, symmetry, deformity, edema and crepitus.
When a muscle, tendon or ligament has been injured, often blood vessels are ruptured spilling blood into the tissues – which has to go somewhere and can migrate between tissues and come out under the skin in areas a bit remote from the broken vessels. (Bruising shown in photograph of sprained ankle).
In treatment, we use the mnemonic “RICE” which stands for “rest,” “ice,” “compression” and “elevation” just like we advise you to do at home. Sometimes, based on our examination, we might want to extend to things like air-splints or plastic/Velcro braces.
Sports trainers use ankle taping which provides support while still allowing some motion; HOWEVER, we’ve found that the effectiveness of taping is HIGHLY DEPENDENT on the skill of the person applying the tape and is therefore often not successful.
In the case of most ligament injuries it is just as critical to improve range of motion during healing as it is to treat the pain. It’s highly important to allow the ligament to heal without reinjury or the resulting laxity will predispose to recurrent sprains.
Heat and Sun-related Illness
We call injuries related to the sun or other sources of heat – thermal injuries; and, for the most part, they are preventable. These are things like sunburn, heat cramps, heat exhaustion and heatstroke.
Because children are less capable of sweating than adults it is harder for them to cool off! Which, of course, makes them exquisitely more susceptible to these injuries and more difficult to treat.
Heat cramp is the most common of sport’s injuries and consists of intense muscle spasms after exercising long enough to have lost large amounts of fluid and salt – which, as I said, is surprising in just how quick it can happen in the heat.
They are a mild form of heat illness which can usually be easily treated by removing the child from activity, and placing in a cool area with no sun exposure. Provide water and food or a sports drink containing electrolytes to help replace fluid and sodium loss; BUT, do not give caffeine. Light stretching, relaxation, and ice massage of the cramped muscles may also help.
On the other hand, heat exhaustion and heatstroke are life-threatening and no laughing matter. Expert treatment should be rapidly obtained and assessment for transport to an emergency facility.
Heat Rash – “Prickly Heat”
The body can do other odd things in response to continued heat. For example, some people are genetically predisposed toward blocked sweat glands if the heat causes them to be over-worked. The rash in the photo to the left is highly pruritic and the person is very uncomfortable.
Treatment is to get out of the sun and heat and to keep the area dry. Unless continually aggravated, the rash usually resolves in a few days. Occasionally anti-itching medications are used.
Persons susceptible to heat rash will have it over again during exposure to heat, so soon learn methods of limiting such exposure – even which sports cause it the worse.
Heatstroke
Because they are so dangerous, we must mention heat exhaustion and heatstroke in this list of summer trauma. “Exhaustion” can sometimes occur “on the way to stroke” but doesn’t need to. Both are caused when fluid and electrolytes lost through perspiration are NOT REPLACED and dehydration ensues with weakness, fatigue, dizziness, fainting, nausea and vomiting being the earliest, and least dangerous, symptoms.
Immediate rest, cooling and replacement of fluids and electrolytes may ward off the development of full-blown heatstroke; but, often, once the process begins, it tends to make itself worse in many ways and becomes increasingly difficult to correct.
Once the body temperature exceeds 41°C (106°F) the brain becomes cloudy and full heatstroke has arrived – medical treatment must be immediately obtained. The body has now lost its ability to cool itself through sweating (because there is no more fluid to loose) so core temperature rises even further. Death is imminent without treatment.
Existing dehydration, fatigue, poor fitness, and lack of acclimatization to the heat are all predisposing factors to heatstroke.
Water should always be available to athletes in order to replace evaporative losses and much effort has been made to educate coaches about procedures and precautions to follow when practicing or playing in the heat.
Immediate cooling is needed. Cold water immersion is safe and is the best choice. When the heat increases, coaches should have the equipment needed for noninvasive cooling at hand – including ice, water, and a large plastic bag and tarp. Believe me, a doctor in the ER would become much more invasive with methods of cooling.
Humidity and Heat – a Double-Whammy
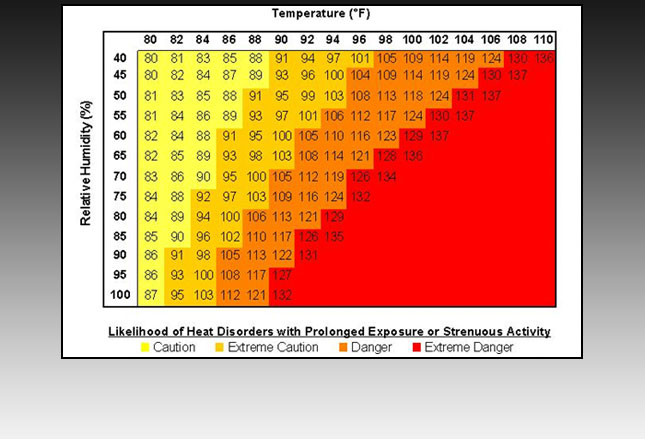
Similar in concept to the “wind chill factor,” but exactly opposite, we have a chart which lists how hot a given temperature “feels” when the atmosphere is at different humidity ranges. Evaporation, the leading cooling method, doesn’t work well when the humidity goes up.
Humidity going up means that the ability to loose heat through sweating goes down – dramatically; therefore, the risk of heat-related illness skyrockets.
It’s clear from the chart that when it’s only 90 degrees, humidity of only 40% (both extremely common in US summers) throws children’s activities into the EXTREME CAUTION zone. At 60% humidity (common in the south) it takes less than 2 more degrees (over 91) in order to throw children’s activities into the DANGEROUS zone.
Really, what is the point of children continuing to exercise competitively AT ALL when heat is anywhere in the EXTREME DANGER zone?! Remember, this is children’s sports we’re talking about. There is no GAME in the world worth the risk – even a sports one!
Rules For Children’s Sports In The Heat
⇒ Children must receive a 5- to 10-minute rest and fluid break after every 25-30 minutes of activity when the temperature climbs past 98°F.
⇒ Additionally, at this temperature, when the humidity rises above 55%, children should be in shorts and t-shirts wearing only helmet and shoulder pads.
⇒ Once the humidity rises past 80%, children should remove all protective equipment during activity.
⇒ When the temperature is over 98°F and the humidity is 100%, coaches and trainers should cancel or postpone all outdoor practices/games (or before). Such activities must be moved into an air-conditioned space if they are to be held.
Traumatic Brain Injury (TBI)
We call it “Traumatic Brain Injury” (TBI) now instead of merely the name “concussion.”
First, it’s because we never quite got the definitions together under the old name; and second, it tells us clearly that concussions are part of a much, much bigger picture which we’ve just begun to understand.
TBI is any insult to the head or body which disrupts the normal function of the brain – in any of its responsibilities – and most are mild (the new definition of concussion).
In concussion TBIs the actual injury(s) is functional (the processes) and not structural (visible damage to tissue) – at least that we are currently able to see.
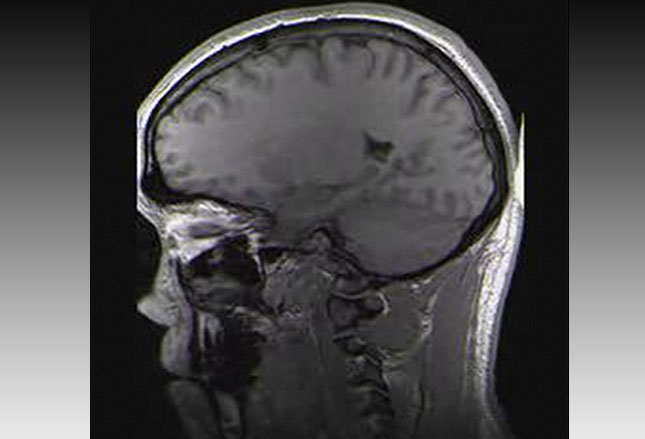
So, no abnormality is usually seen on current CT or MRI scans even though testing can clearly show that there must be some damage somewhere – or the brain wouldn’t have quit working normally.
There are 250,000 children treated in ERs every year for sports injuries whose diagnosis includes TBI or concussion. Of those under 14 years old, 55% have been caused by falls; and the leading cause of those that die is motor vehicle accidents.
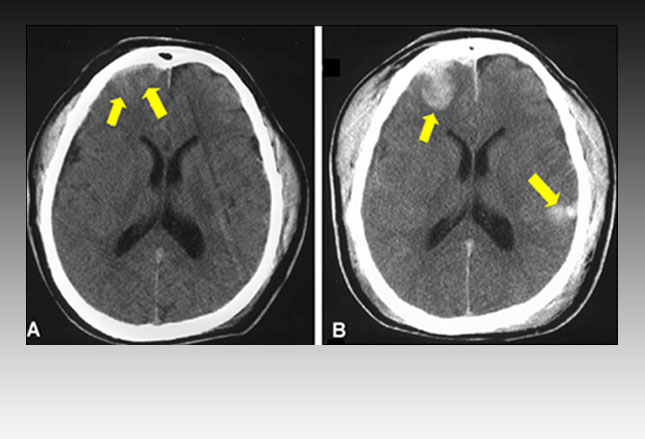
The photo on the right, above, shows a CT scan containing multiple areas of structural damage and bleeding (brain contusions and hemorrhages) in the most common areas – the frontal and temporal lobes.
TBI–Concussion
We’ve said then that the diagnosis of “TBI–concussion” is largely by clinical experience and some testing (although, in order to rule out full TBI some type of imaging test would usually have already been performed, like that in the photo to the left).
Additionally, the type of experienced clinical exam and testing necessary to diagnose a TBI–Concussion is usually NOT available on the field of children’s sports venues; which leaves the expert handling of children up to the integrity and good judgement of coaches and trainers.
Hopefully, they also have a healthy added dose of parental-type worry and caution because TBI–Concussions can have long-term effects… very, very long term.
Four categories of concussion symptoms exist: problems with thinking/remembering, physical problems, problems with emotion/mood and problems with sleep.
Patients we see might only claim a headache and/or dizziness or unsteadiness. Although, if a doctor chooses to spend the time necessary, there is usually evidence of difficulty concentrating, amnesia, blurred or double vision, drowsiness and/or irritability. Remember, diagnosis is clinical based on a thorough systematic evaluation and much confusion in the past has been due to inadequate evaluation/examination as well as patient dishonesty in a mistaken desire to continue playing.
We’ve only discovered just recently how critical not only physical rest but mental/cognitive rest is for full recovery and avoidance of re-injury.
If physicians don’t have either the ability, training, desire, time or equipment capabilities to diagnose, test, monitor and treat concussions, referral to a concussion specialist is important – especially for persistent, severe and/or changing symptoms.
Commotio Cordis
It was only the deaths and disabilities of professional athletes with TBI that pushed this next issue off the front page for sport’s injuries: Commotio Cordis
This odd sounding name is the sudden, unexpected death of an athlete when struck in the chest on the court or field – like by a ball or helmet or something. A rare but unsettling event that always makes the headlines, especially in a child, like lightening striking twice in the same place.
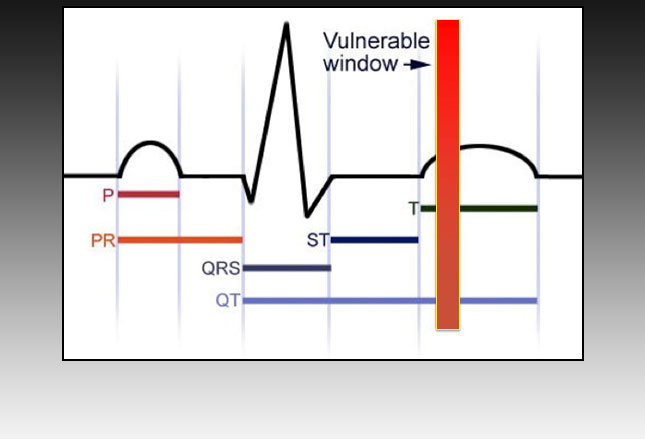
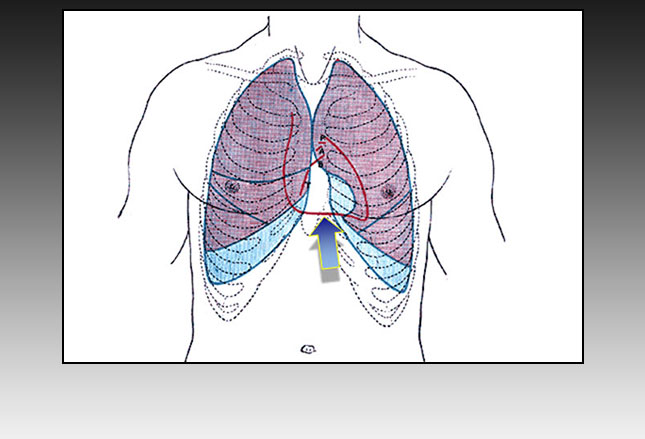
You see, IF a susceptible athlete recieves a striking blow to an area just to the left of the breast bone, between the second and fifth ribs (blue arrow below) AND IF it occurs in the 10-30 milliseconds at the beginning of the “T” wave (repolarization) in the cardiac cycle (red bar on the right) THEN that athlete is vulnerable for instant death by unexpected heart attack.
The whole cardiac beat cycle being only 1000 milliseconds, needing to hit a tiny window of only a 2% portion explains why commotio cordis is such a rare event. Rare but not unheard of.
The number of cases each year is right up there with Hypertrophic Cardiomyopathy (HCM); but, unlike HCM, it cannot be picked up ECG testing beforehand – to do that you’d need a crystal ball.
We used to think that only 5% of kids survived cordis but now some data seems to be in the neighborhood of 60%; so, we don’t really know what to think. Except that we do know that chest protectors merely reduce trauma not offer absolute protections; because a third of the victims were wearing protectors!
For doctors, we consider cordis a diagnosis of exclusion because we must rule out a host of other things first (like electrolytes, heart attack, HCM or fibrillation). There is no special treatment that we know about over and above the prompt recognition, resuscitation and defibrillation we normally use.
Exercise-induced Asthma (EIA)
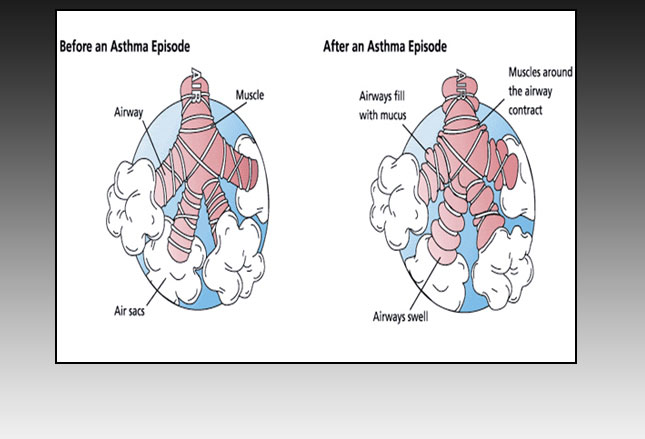
People often think of “Asthma” as being only a problem with “allergies” like pollens and dander. Not so! Exercise triggers a form of asthma too!
It’s called: Exercise-induced asthma (EIA) and it’s triggered by the loss of moisture in the airways when you breath faster or from the cooling of the airways from the large volume of outside air that is cooler than the body temperature.
We’ve discussed before that the “real culprit” is the “atopy” which people are born with causing them to be more sensitive to intrusions (triggers) and a whole lot more aggressive with their bodies defense system against it.
In the case of EIA, once the attack is triggered, bronchospasm, edema, and mucous production and plugging ensue. Sometimes kids can have “regular” asthma and EIA together, sometimes only EIA alone and sometimes it’s only to specific types of exercise (i.e. running not swimming) or environments (i.e. swimming pools not ice rinks).
All treatment must be specifically tailored to every child. Sometimes only short-acting bronchodilators before exercise is needed; sometimes a different “preventive inhaler” is used; sometimes we merely switch sports; sometimes we need to be more vigorous with the “regular asthma” to decrease the sensitivity to exercise “triggers.”
Tinea corporis (ringworm)
Perhaps you remember having this (and the next item) from your own gym class. It’s very common and spreads by both skin-to-skin contact (i.e. wrestling) and shared clothing or equipment.
As a contagious fungal skin infection, the skin is usually itchy and scaly. It usually easy to treat with antifungal creams both over-the-counter and prescription. It is prevented by wearing loose-fitting clothing made of cotton or synthetic materials; as well as by NOT sharing clothing, gear or towels.
Tinea pedis (Athlete’s Foot)
Similar to ringworm above, athlete’s foot is caused by a fungus too. Just a different type.
And the skin, of the foot and toes, becomes scaly and itchy too, with the addition of the sensations of “burning” and “stinging” along with some redness. It is treated with over-the-counter medications but often does need a prescription for antifungal medicines.
It can be a bit difficult to treat (resolve) largely because of the difficulty identifying the specific “trigger” or “reinfecting” agents. Sometimes it’s the “plastic” shoes. Sometimes the “colored” socks or type of material. Sometimes it’s the poor cleanliness of athletic equipment or shower grout, etc., etc..
For protection, children should wear foot protection (eg, sandals) in locker rooms and bathing areas, keep their feet clean and dry, and wear shoes that are well ventilated and made of natural materials.
Staphylococcus Aureus Infections
Being an athlete (hot, sweating, surface contacts) makes you more vulnerable to cuts and abrasions turning into full infections. Just being a child does the same thing. Being BOTH is a “double whammy” and even the tiniest of scratches can turn into full-blown boils or cellulitis – usually from Staph Aureus (not the “good” kind).
This bug is becoming an increasing public health concern because it’s the one that often can’t be treated well, which we’ll talk about in next section.
Children are at particular risk of developing a Staph skin infection if they have an abrasion, cut, or bug bite; attend daycare centers or school settings; and come into contact with others in locker rooms and workout facilities. Shared towels and equipment are a haven for bacteria.
To prevent infection, children should wash their hands often with soap and water for a MINIMUM of 15 seconds or use alcohol-based hand sanitizers/wipes; avoid sharing bar soap, towels, razors, uniforms, and other items that touch the skin; and EVERYONE needs to keep their wounds and sores covered.
Treatment may involve incision and drainage (I&D) of the abscess and/or appropriate antibiotic therapy which is based on local susceptibility rates.
MRSA Infection
For many reasons our culture is now faced with what is known as “antibiotic-resistant bacteria” in ever more common situations. Your children might have been at too tender of an age to have been told that their beloved “Kermit the frog” (Jim Henson) actually died because of antibiotic-resistant bacteria (also treated late).
Athletes competing in contact sports are at much more risk of developing a Methicillin-resistant Staph Areus (MRSA) infection than he was manipulating puppets.
In early stages, an MRSA skin infection is often confused with a rash, pimple, or a spider bite because the symptoms are similar: red, swollen, warm, or tender. Over 48 hours though, the affected area frequently becomes more painful and swollen; but, how would a lay person know that unless they’d seen a number of cases before?
Often, an abscess will develop underneath the skin. Occasionally, this abscess begins to drain on its own; at other times, I&D of the abscess is required. When a cellulitis spreads or does not improve after 2-3 days on routine antibiotics, it may be MRSA.
MRSA is resistant to many antibiotics, frequently requires specific antibiotic treatment and often in an inpatient setting.
Hymenoptera Stings
Let’s end this lengthy treatise with stings. They are at least as common to athletes these days as MRSA infections and can be just as debilitating and deadly.
Taking place outdoors in warm weather, sports are particularly common locations for bees, wasps, yellow jackets, hornets and ants (at least in the U.S.) – all known as Hymenoptera.
Making these fellows upset, as flailing-about-players often do, results in swelling and other symptoms, such as redness from the sting or bite that may last a week or more, nausea, fatigue, and low-grade fever.
More commonly now than before, stings can result in a life-threatening anaphylactic reaction with difficulty breathing; hives; swelling of the face, throat, or mouth; rapid pulse; dizziness; or a drop in blood pressure. For those who are severely allergic, epinephrine should be administered immediately after a sting, and the patient should be rapidly transported to the closest appropriate medical facility.
In the absence of a severe allergic reaction, the stinger should be removed, site cleaned and ice applied to reduce swelling. Oral antihistamines may reduce itching and ibuprofen or acetaminophen may be used for pain relief.
That’s all I can think of for now and thanks for hanging in here with me… you’re a good person. Fore-warned is fore-armed.
2 Posts in Sports Injuries (common-sports-injuries) Series
- Sprains to Infections – 14 May 2016
- Common Fractures – 10 May 2016
Advertisement by Google
(sorry, only few pages have ads)