Innocent Heart Murmurs in Children
The term “Innocent Heart Murmur” sounds anything BUT innocent to most parents; but, it’s not an uncommon “diagnosis” for a pediatrician who is actually doing a thorough exam of a youngster.
However, just like nearly everything else in the physical exam a doctor performs, there is a significant variability in what your doctor may look at, or pay particular attention to, during the exam. It depends on his/her training, particular interests, and probably most importantly the clinical setting and what he is looking for.
What a doctor calls a “murmur” is a vibratory noise of some sort that is heard with his stethoscope when listening to the chest, neck or abdomen. A Pediatrician (physician specially trained in children’s diseases) spends many years of training learning to recognize the usual sounds which are “supposed” to be in a child’s chest and how they sound at each age during growth: breath sounds and the various heart valves slamming open and shut.
Being able to do that makes all the unusual things stand out to be recognized. Then, of course, there are all the interfering sounds of a squirming child, gurgling bowel, rustling clothes (if you haven’t removed all the shirts) and background noises of people talking. A lot to try and “tune out” if you’re not careful, making it very easy to miss something important.
However, if you’re successful at the task, what that leaves for you to hear are all the sounds associated with moving the blood through the tubes and around the body. Oh, and the slight changes in the timing, location and quality of the “normal” things that might be giving clues about any changes in pressures or muscle firings going on inside.
 I’m going to list some of the “innocent” things your doctor should be listening for and what they mean, there are quite a few; so, that should put your mind more at ease if your doctor uses the term in reference to your child. All that said, however, the stakes are high because a murmur in a child is often the sole indication of a serious heart disease and none of us want to miss one of those.
I’m going to list some of the “innocent” things your doctor should be listening for and what they mean, there are quite a few; so, that should put your mind more at ease if your doctor uses the term in reference to your child. All that said, however, the stakes are high because a murmur in a child is often the sole indication of a serious heart disease and none of us want to miss one of those.
General Heart Exam Principles
I’ll tell you a secret. If your doctor is having to “work around” any of those distractions I’ve listed above – there is a greater chance he could miss something. You REALLY want your doctor to listen to your child’s heart with shirts completely removed, in a quiet room and holding still. So, that’s the first thing a parent should know about the “heart” portion of a child’s exam and it’s up to you to try and help make it happen.
Another principle is that heart sounds dramatically change as the child grows. That means that even though a doctor didn’t hear one before, the child may have one now because things have changed inside the chest. This is particularly true in the first year or so of life but can occur well into adolescence – so you really don’t want to miss one of those “well baby checks.”
I’m going to assume that you already know a few things about the heart from your high-school health class like that the heart is triggered to pump when an electrical pulse begins at the atrial chambers and spreads through the ventricles; and that there are four valves which first open then slam shut at each pump – the systole. Also that there is a rest period where the heart can fill with blood again – the diastole; and that the two phases together are what is called a “cardiac cycle” which generates an audible sound: “Lub – Dub.”
“Lub” is mainly the sound of the two main high-pressure inlet valves slamming shut during the “pump” and “Dub” is the two smaller “back-flow prevention” valves shutting at the beginning of the “rest” portion. Normally a doctor does NOT hear either valves opening or any other sounds like the blood flowing. [The squiggly lines on the chart at the side represent sounds that the doctor hears in his stethoscope]
Physical Examination for Murmurs
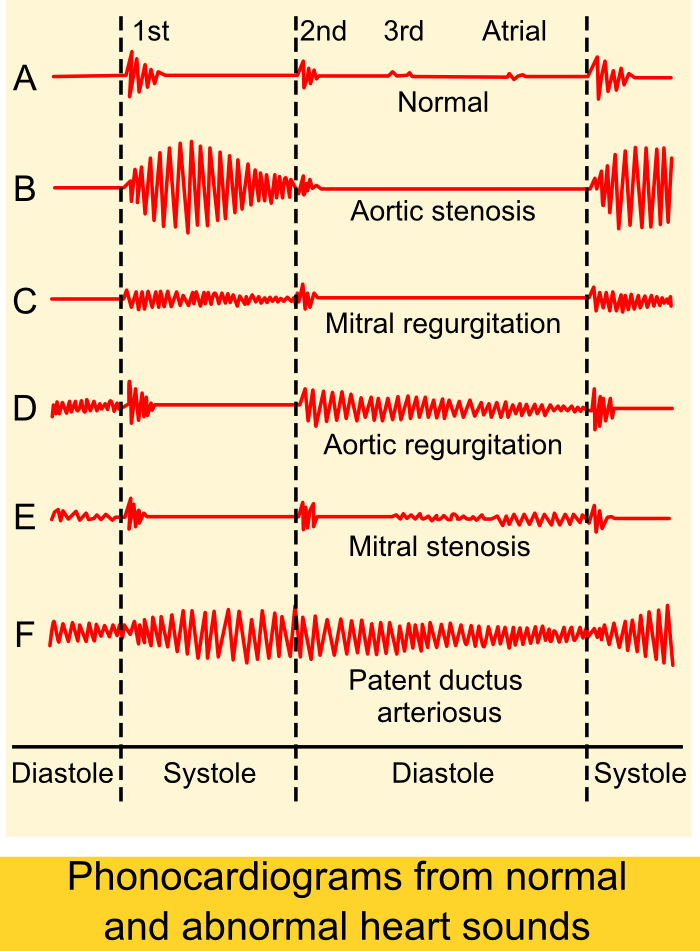 If there is a problem with one of the valves, or a roughened surface, or a hole in one of the partitions then extra sounds start occurring which the doctor must try and explain.
If there is a problem with one of the valves, or a roughened surface, or a hole in one of the partitions then extra sounds start occurring which the doctor must try and explain.
To explain a murmur the doctor will begin to focus on the child’s vital signs; exercise capacity (for age); side-effects, if any, in the chest or abdomen; and a thorough cardiovascular exam including feeling pulses, feeling the chest and back, and listening to the heart until he can put everything he hears into words.
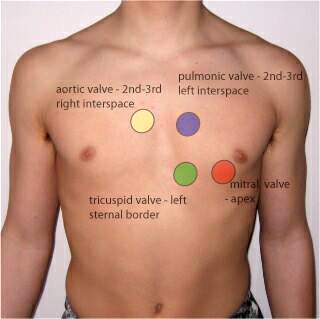
If you are watching closely you will see the doctor listen carefully to at least four locations on the chest for several heart pumping cycles each and use both sides of his stethescope. You will see him feel pulses while he listens and have the child turn on his side then stand up in order to listen again.
He will listen again after the child does a little exercise and may also have him squat. All of this so that he can hear the heart from every angle and see what happens when position and rate changes.
Medical Description of Murmurs
Intensity: A murmur can be soft (grade 1) or loud (grade 6) or several grades in between. Grade one is barely audible; 2 is faint but can be heard immediately; 3 is moderately loud; 4, heard in a wide area but cannot be felt on the chest; 5, loud and can be felt (a thrill); and grade 6 murmurs are loud enough to hear with the stethoscope raised off the chest.
In addition, the pitch and/or intensity can change during the cycle giving a “crescendo,” “decrescendo,” or “ejection” type murmur.
Location: Murmurs reflect the location over the heart that they are heard loudest and are usually described in reference to the sternum: upper-left, right, lower-left, etc.. They may also radiate in some direction, such as: “Heard along the left sternal border and radiating to the back.”
Duration: They may be short – meaning they don’t exist during a whole systole or diastole; or, they may be “holo-systolic” – i.e. covering the whole systole. Or, they can even cover both the systole and into diastole.
 Quality: Murmurs also have a “quality” to them, using such descriptive words as: “harmonic,” “high-pitched,” “harsh,” or “musical.”
Quality: Murmurs also have a “quality” to them, using such descriptive words as: “harmonic,” “high-pitched,” “harsh,” or “musical.”
Associated sounds: And lastly, there are other sounds made by stiffened muscle, stenotic valves or other things which doctors use to “troubleshoot” problems with the heart such as: “clicks,” “gallops,” or “rubs.”
All of these descriptions have significant meaning to doctors and nurses and give tell-tale signs of what, if anything, may be going wrong.
What your doctor may say to you could be: “He has an innocent heart murmur that we’ll need to follow but may eventually disappear entirely.”; and what he might write in the chart might be: “Grade 2/6 harmonic ejection murmur heard best along LLSB without radiation or changes in position or exercise.”
Differentiating Types of Murmurs
The “red flags” that doctors look for when they are diagnosing a murmur are: a murmur which is holosystolic or diastolic, a grade 3 or higher, of harsh quality, associated with an abnormal second heart sound, has maximal intensity at the upper left sternal border, associated with a systolic click or one that is louder when the child stands up.
There is an increased likelihood that the murmur is one of the pathologic ones if any of those things are heard.
On the other hand, an innocent murmur is more likely if: it is only systolic, is soft and difficult to hear, is of short duration, is harmonic or low pitch, varies in intensity with phases of breathing and posture (louder when laying down) or which become louder with exercise, anxiety or fear.
The most common innocent murmur is what is known as a “Still murmur”, which is characteristically loudest at the lower left sternal border and has a musical or vibratory quality that is thought to represent vibrations of the left outflow tract.
 If a general physician, or even a board certified pediatrician, hears any of those “red flags” a consultation with a pediatric cardiologist should be obtained. He will most likely perform an Echocardiogram (especially in infants) which should give a definitive diagnosis. We don’t use x-rays and ECGs so much any more.
If a general physician, or even a board certified pediatrician, hears any of those “red flags” a consultation with a pediatric cardiologist should be obtained. He will most likely perform an Echocardiogram (especially in infants) which should give a definitive diagnosis. We don’t use x-rays and ECGs so much any more.
Types of Innocent Murmurs
Why am I telling you all this? Well, because it’s interesting AND I’d like you understand that there are several types of innocent murmurs all with different descriptions and all shown not to interfere with a child’s growth or development.
In addition, so you know that there are way more “innocent” murmurs heard in children than “pathologic” ones (the ones which can mean a problem).
Your pediatrician (and family practioner) will (should) refer you to a pediatric cardiologist any time that they cannot say with certainty the murmur or sound is innocent. And he/she should be referring at a level to be “safe rather than sorry,” i.e. many referred children will be adjudged to have innocent murmurs.
Innocent Heart Murmurs – Hard Description
| Type | Description | Age at detection |
|---|---|---|
|
Aortic systolic murmur |
Systolic ejection murmur best heard over the aortic valve |
Older childhood into adulthood |
|
Mammary artery soufflé* |
High-pitched systolic murmur that can extend into diastole; best heard along the anterior chest wall over the breast |
Rare in adolescence |
|
Peripheral pulmonary stenosis |
Grade 1 or 2, low-pitched, early- to mid-systolic ejection murmur heard over axilla or back |
< 1 year |
|
Pulmonary flow murmur |
Grade 2 or 3, crescendo-decrescendo, early- to mid-systolic murmur peaking in mid-systole; best heard at the left sternal border between the second and third intercostal spaces; characterized by a rough, dissonant quality; loudest when patient is supine and decreases when patient is upright and holding breath |
All |
|
Still murmur |
Grade 1 to 3, early systolic murmur; low to medium pitch with a vibratory or musical quality; best heard at lower left sternal border; loudest when patient is supine and decreases when patient stands |
Infancy to adolescence, often 2 to 6 years |
|
Supraclavicular\brachiocephalic systolic murmur |
Brief, low-pitched, crescendo-decrescendo murmur heard in the first two-thirds of systole; best heard above clavicles; radiates to neck; diminishes when patient hyperextends shoulders |
Childhood to young adulthood |
|
Venous hum |
Grade 1 to 6 continuous murmur; accentuated in diastole; has a whining, roaring, or whirring quality; best heard over low anterior neck, lateral to the sternocleinomastoid; louder on right; resolves or changes when patient is supine |
3 to 8 years |
Innocent Heart Murmurs – Easy Description
This is how we learned it in medical school using the nemonic of “The Seven S’s of Innocent Murmurs.”
- Sensitive (changes with child’s position or with respiration)
- Short duration (not holosystolic)
- Single (no associated clicks or gallops)
- Small (murmur limited to a small area and nonradiating)
- Soft (low amplitude)
- Sweet (not harsh sounding)
- Systolic (occurs during and is limited to systole)
This is a fairly complete description of innocent heart murmurs. Perhaps more than you wanted to know; but, now you’ll know what to expect and how to understand what your doctor is doing/saying when discussing that he hears a murmur in your child.
[Am Fam Physician. 2011 Oct 1;84(7):793-800; http://www.aafp.org/afp/2011/1001/p793.html]
Advertisement by Google
(sorry, only few pages have ads)

