Emergency Medical System (EMS) – Prevention
Just ask anybody. With all the gadgets and technology we have now, most children are saved in emergencies, right? All the television shows prove it, right? Now days, just call 911 and paramedics save most children… right?
WRONG! It is true that, for adults, the EMS system has dramatically improved survival; but, for children the survival rates in out-of-hospital cardio-pulmonaryarrest are abysmal.Survival, ranges from only 3% to 17% in most studies; and, survivors are often neurologically devastated- as high as 50%.
Even in this day and age a child in arrest is far-and-away more likely to die than livewhen the EMS system is activated, than live. Why is that? A whole lot of reasons, but mostly because very few pediatric cardio-pulmonary arrests are due to heart attacks. It turns out, apparently, that adult heart attacks are more easily treated than almost all of the reasons children’s hearts stop beating.
In children, most cardiopulmonary arrests occur around the home; and SIDS, trauma, submersion, poisoning, choking, severe asthma, and pneumonia are the most common causes.
The differences are so pronounced that the EMS procedures have needed to be altered for children, the: “EMS-C: — the Emergency Medical System for Children”
In adults most sudden, nontraumatic cardiopulmonary arrests are cardiac in origin and it’s usually ventricular fibrillation or other ventricular tachycardia. The single best thing to do in that case is to "shock" or defibrillate… so, in ADULTS call 911 first because they can bring the machinery to do it.
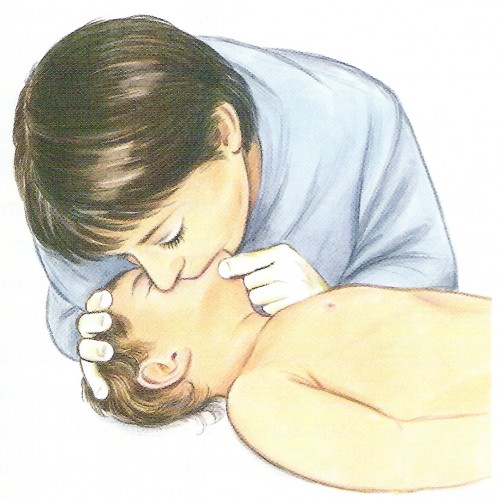
In children, most cardiopulmonary arrests occur around the home; and SIDS, trauma, submersion, poisoning, choking, severe asthma, and pneumonia are the most common causes. The breathing has gotten progressively worse until it causes unconsciousness and the heart to stop. Defibrillating is rarely needed… so, in CHILDREN start CPR first for one minute, before calling 911.
Because most pediatric arrests are secondary to progressive respiratory failure, immediate CPR (i.e. phone fast rather than phone first) is the default approach in the pediatric "chain of survival."
If there are two people with the dying child it makes it a lot easier, just do both things at once- call and resuscitate.
To simplify the message to the lay public, the adult sequence (phone first) and techniques are used for victims 8 years of age and older in the out-of-hospital setting and the child sequence (resuscitate for a minute first) is used on children under eight.
There are incidences when the "children’s protocol" (EMS-C) should be followed even for adults; namely: arrest caused by drowning, trauma and drug overdose. Likewise, if a previously well child has just suddenly collapsed without apparent cause, or if the child has known cardiac illness then the adult, call first, approach should be used. However, just to simplify the message to the lay public, and make it easier to remember, the adult sequence (phone first) and techniques are used for victims 8 years of age and older in the out-of-hospital setting and the child sequence (resuscitate for a minute first) is used on children under eight.
BUT, take a GOOD look at the leading causes of cardiopulmonary arrest in children. I’ll mention them again: SIDS, trauma, submersion, poisoning, choking, severe asthma, and pneumonia. Notice anything? MANY if not MOST of them are PREVENTABLE!
You can do more to prevent your child from dying by being meticulous about prevention issues, than you ever could by going to medical school and carrying a bag full of resuscitation drugs
That’s why the EMS-C lists "prevention" as the first link in the "pediatric chain of survival." Have you heard so much about children’s safety that you tend to gloss over it? Do you think that calling it "the FIRST link" is a "soft," unrealistic approach, or a bit of an exaggeration just for effect?
If so, go back and re-read paragraph two. Way less than 17% of children who arrest don’t make it!! Believe me when I say that you can do more to prevent your child from dying by being meticulous about prevention issues, than you ever could by going to medical school and carrying a bag full of resuscitation drugs with you at all times!
Those silly, nagging, tree-hugging, obnoxious, all-over-the-place people who have forced seat belt legislation, helmet laws, safety lids, air bags and the like on us have saved more children than EMS paramedics! Still think it’s not important?
I AM going to teach you about the things you should know of CPR; but, first will you keep reading if I tell you about the list of "prevention" issues mentioned in the Pediatric Advanced Life Support (PALS) provider manual which we pediatricians need to know to re-certify? Cause these are where the money is at, for you.
READ THESE over and over, until you can honestly say you have put all of them into practice! This is where children’s CPR Begins!
The goal is to limit the most frequent injuries or illnesses for which there are prevention strategies available. The leading cause of potentially preventable death in infants (1 to 12 months) is SIDS, in children (1 to 24 years) it’s injury; namely, motor vehicle, pedestrian, bicycle, submersion, burns and firearm.
Reducing the risk of SIDS The unexpected death of an infant (under 12 mos), without other apparent cause, is called SIDS. There are many different causes, not all of them known, but two that come to mind are: botulism toxin, and rebreathing asphyxia.
Some years ago it was discovered that some infants given honey as a sweetener to food unexpectedly died. Actually, it took a great deal of work to discover that it was dormant botulism spores found in some honey which, when ingested in an infants immature gut, developed toxin that caused death. So DO NOT add honey to any infants formula or food.
Fairly recently it has been shown that SIDS occurs more frequently in infants who sleep prone (on their stomach) than those who sleep on their back or sides. Especially if placed on soft, fluffy surfaces like lambs wool, comforters or other surfaces which might trap exhaled air near the face, infants can suffocate by re-breathing "stale" air low in oxygen and high in carbon dioxide.
This "back to sleep" public education campaign was introduced in the US in 1992 and has been associated with a more than 50% reduction of SIDS nationwide.
Other associations which have been noted in SIDS deaths are: winter months, lower family income, male gender, a mother who smokes cigarettes or is addicted to drugs, a history of apparent life-threatening events, and low birth weight. Stopping cigarette smoking of any kind around infants may be the next great attack for saving their lives!
Child in Car Seat
Prevention of Motor Vehicle Injuries These account for almost half (50%) of all pediatric deaths! Half of those could have been prevented by appropriate use of seat and shoulder restraints! Since 1987 air bags have saved more than 5000 lives in the US. Unfortunately there were 74 children killed by airbags; but, most of them were either improperly restrained for their age or not restrained at all.
Adolescent drivers are responsible for a disproportionate number of motor vehicle-related injuries and, surprisingly, drivers education classes have not only increased the number of adolescent drivers at risk but there has been no improvement in safety. Half of their fatalities also involve alcohol!
Prevention of Pedestrian Injuries A leading cause of death among children 5 to 9, they occur when a child darts into the street between intersections. Roadway lighting, construction of sidewalks and barriers must be pursued as "passive prevention devices."
Prevention of Bicycle Injuries Two hundred thousand injuries and 600 U.S. deaths each year are from using bicycles. Bicycle helmets reduce the severity of head and brain injuries by around 85%, do your children ride without them?
Prevention of Submersion and Drowning Internationally these are responsible for 15% of injury deaths under 14 years of age. No one should swim alone especially children. A pool that is not completely surrounded by a secure fence with a locked gate is significantly dangerous to a child under 5.
Children older than 5 should learn to swim but even supervised children should wear personal flotation devices when playing in rivers, streams or lakes.
For adolescents alcohol is a significant risk factor for drowning injuries and deaths.
Prevention of Burn Injuries 80% of fire and burn related deaths are from house fires, most in private residences, usually without smoke detectors. Smoke detectors are the most effective intervention for preventing death from burns and smoke inhalation and can reduce death and severe injury by 86% to 88%.
Smoke detectors should be placed, and checked regularly, outside of sleeping and napping rooms and at the top of all stairways. Also have a discussion, andeven role play, with your children about evacuation procedures.
Prevention of Firearm Injuries Most guns used in childhood unintentional shootings, school shootings and suicides are from the home. Thirty-four percent of high school students surveyed reported easy access to guns and an increasing number of children carry guns to school.
The mere presence in the home is associated with an increased likelihood of adolescent suicide. Firearm homicide is the second-highest cause of death among all adolescents and young adults in the US, Norway, Israel and France and the highest among African-American’s.
They should be stored in a locked container and unloaded with a trigger lock in place. Ammunition should be similarly stored locked up but in a different place than the gun.
Prevention of Choking More than 90% of deaths from Foreign Body Airway Obstruction (FBAO) are in children under 5 and 65% are infants. The incidence had decreased significantly with toy legislation. But toys, balloons, small objects and foods (hot dogs, round candies, nuts, seeds, grapes and popcorn) still cause FBAO.
Always stop and correct children who attempt to eat while running or other play activities as that is when risk of choking is highest.
Now, I promise that I will talk about CPR in another article. I hope you agree that reading this has been worth it. If you have considered and taken care of all of the above categories to the best of your abilities- you are probably 1 in 1,000. It is no wonder that the US has the second highest death rate in children (14/100,000)- out of all the developed countries participating in the international collaborative effort- second only to New Zealand (who “beat” us in vehicle and drownings 17/100,000).