Refresh: 15 Back To School Diseases
I’ve written about back to school diseases and problems before but it seems that questions and issues just keep the topic alive and asking for an update.
This will be just a quick update of 15 back to school diseases your child may encounter now that school bells are ringing again.
Reason NEVER to share a hairbrush (Click for action)
Back To School Diseases
Refresher course of “school-born” medical problems
Now that our kids are back in the classroom there is a new element we must consider in our discussion about the spread of illnesses around the community: epidemiology—the study of how diseases spread around the community
It’s important, for example, because your elementary aged children not only have 20-50 new “close contacts” (depending on the school district) they also now are dealing with, perhaps, hundreds of secondary contacts like lunchroom staff preparing their food, other students/classes on the playground, classmate’s parents and siblings and all the friends of those.
The classroom is a breeding-ground for organisms and “things” which cause illness – like the lead louse on the brush seen in the photograph… and there are others. Look at the photos below to refresh your memory.
Pediculus humanus capitis (Head Lice)
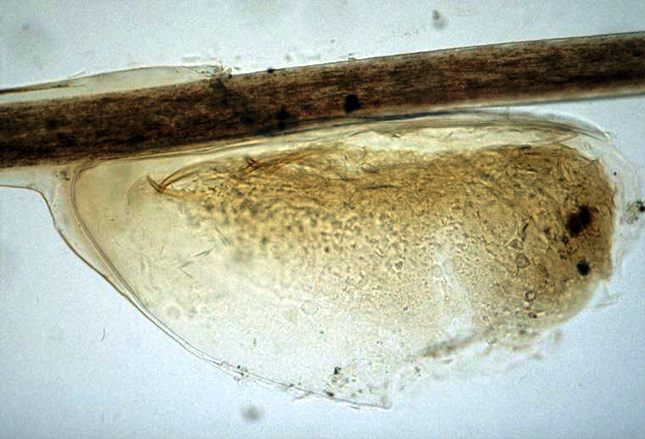
There are a whole bunch of types of lice. The kind we’re talking about here is found on the head, eyebrows and eyelashes almost exclusively and is spread by direct contact with the hair of a person already infested.
Parents and even school personnel can mistake the miniscule parasites for specks of link and even dandruff—it’s easy to do; so, suspected lice should always be confirmed medically by locating a true “nit” on the hair shaft about an eighth of an inch from the scalp.
And don’t think personal hygiene or home/school cleanliness is the culprit for disease spread, it’s not. They are spread by direct contact with the hair of an infected person and less often by contact with some personal items (combs, towels etc.) or clothing (hat, scarf, coat etc.)
“Nit combs” are effective in removal but only if used correctly. Unhatched nits are about an eighth-inch from the scalp so “normal” brushing doesn’t work, you must carefully glide along the scalp with overlapping strokes so as not to miss even a single hair.
And this is one of the rare problems were we DO treat all other household members and close contacts with Pediculicides (medicated shampoos and gels).
Tinea Capitis (Ringworm)

Ringworm is a very, very itchy fungal infection of the scalp which can occur at any age but is nearly always seen before puberty for some reason. There is scaling (usually without inflammation) of the scalp and the hair has a dull-gray discoloration and breaks easily.
A child can get it from the CAT, or a friend, or their personal items with whom/which they have had direct contact—and it doesn’t have to be that great, it spreads easily.
We diagnose the problem by looking at it with a practiced eye, wood lamp (black light) and/or culture; and we treat it with oral medications because topical stuff rubs/washes off to quickly.
Allowed to continue too long and pus-filled sores develop along with fever and swollen lymph nodes. Ringworm can return, even repeatedly if clothing, surfaces, personal items… and pets, aren’t cleaned/treated completely.
Hand-Foot-Mouth Disease (HFMD)

There are a handful of virus types which cause “blisters” on the hands, feet and mouth of children causing, as might be expected, “hand foot mouth disease.” I learned in medical school that the culprit was coxsackievirus A type 16; but, now types 5 and 10 along with enterovirus 71 are in the ring too.
Looking closely, these vesicles are elliptical along the axis of skin lines and accompany fever, skin rash and blisters in the mouth and on the gums and lips. And typically infects children under five.
It’s a virus so is NOT treated with antibiotics and spreads from person to person by contact, air or contaminated objects. Culture an infected person and you find the virus being shed in their saliva, sputum, nasal mucus, blister fluid and even feces.
Treatment is only supportive with mouthwashes, sprays and antipyretics (NOT aspirin)
Scarlet Fever

You see the red lips and coated tongue of this boy but you may not see the swollen tonsils and significant sore throat being caused by Group A Beta-hemolytic Strep (GABS).
Not all cases of scarlet fever have such a coated tongue but when you see it you better look for the red rash somewhere else like the neck, chest, arms, back, abdomen, buttocks, thighs (it often seems to skip the groin). The rash can vary in appearance but pay attention to how it feels, scarlitina (the rash of scarlet fever) feels a bit like sandpaper, rough and slightly raised.
This is how it works: the child (commonly 5 – 12) contracts GABS which causes a fever and sore-throat for a day or so. As the GABS progresses the rash develops and begins to spread, which is known as scarlet fever and scarletina. As the disease wanes the palms of the hands may peel.
If the body has to fully fight off the bacteria on its own without antibiotics the antibodies it developed run the risk of being the type which also attack the heart and vessels; that’s known as Rheumatic Fever (RF). All caused by GBSH in its various manifestations and severity.
That’s why sore throats are cultured and “strep tests” are run; to be able to treat the strep early and try to prevent the body from developing those “rheumatic fever” antigens. These days it’s just a small portion who go on to develop the full RF disease.
Bacterial conjunctivitis (Pink Eye)

The so-called “pink eye” can be caused by both viruses and bacteria. IF caused by a bacteria it is most often due to “H Flu” (no NOT influenza) or “strep pneumonia” (no not the lung kind) and can be treated with topical antibiotics (eye drops).
Those caused by viruses usually depart on their own but occasionally end up getting drops too. The thing is: Pink Eye is HIGHLY contagious! And it is easily spread through families and entire schools.
The eye becomes itchy and red. It tears and eventually drains pus. Frequently children’s eyes are “matted shut” in the morning upon awakening and it often accompanies ear and respiratory tract infections.
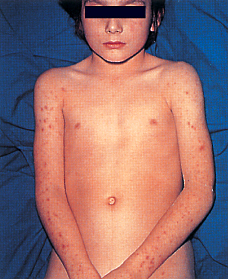
Varicella (Chicken Pox)
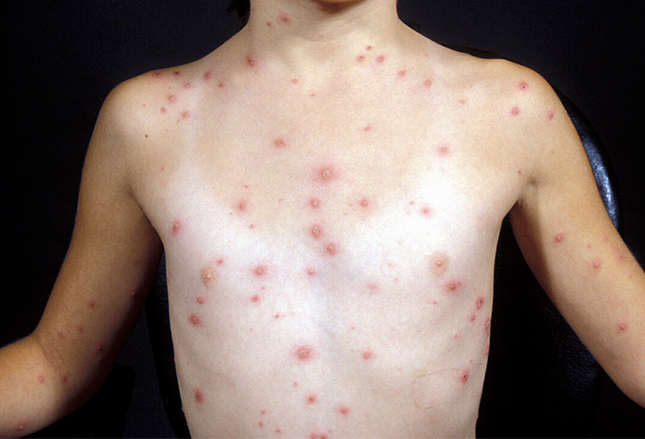
This rash began on the boy’s back and progressed rapidly to his upper arms and chest. Even with the very first “pox” the diagnosis can be made because almost nothing else looks like “A dew-drop on a rose petal.”
Years ago, diagnosing a tiny raised vesicle (blister) on a red base used to be a pediatrician’s claim to fame – along with measles, mumps and rubella, of course. With the effective immunization program of today… not so much.
The “C-pox” is a highly contagious viral diseases caused by the varicella-zoster virus (VZV) which can also lie dormant until it causes shingles in teens, adults and the elderly.
The disease begins with fever and malaise then progresses to the intensely itchy rash which spreads almost everywhere for around a week. Eventually the blisters break and scab over.
And here’s the thing: an infected child can spread their disease to others beginning 2 days BEFORE he/she’s even sick and until the very last pox is scabbed over. That’s sometimes up to two weeks!
Treatment is usually just supportive, and they often need lots of “support” they feel so bad. However, it can be prevented by an immunization— usually given at 12-15 months with a booster at 4-6 years of age.
With immunizations, these days we’ve even got grand-mothers who haven’t seen chickenpox.
Rubeola (Measles)
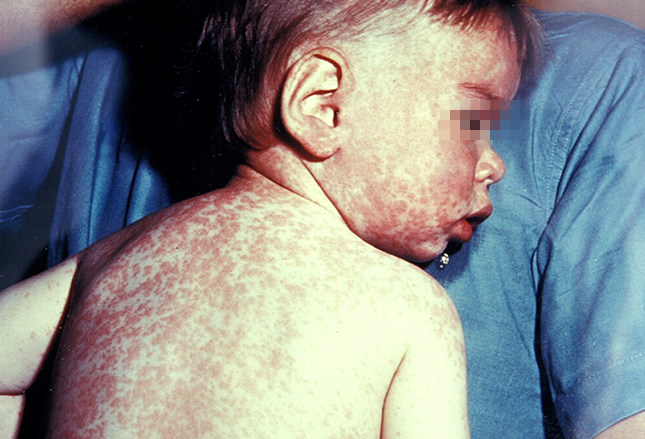
Unfortunately, even in these days of enlightenment, completely preventable diseases like measles continue. The parents of this extremely ill child were confused by the crap on the internet and followed the advice of those claiming “enlightenment” not to accept immunizations.
The baby developed a high fever, cough, congestion, red-mattery eyes and then this rash.
The measles virus can remain active and contagious for over 2 hours IN THE AIR and on surfaces after a sneeze or cough. Just walking through a room where an infected person has coughed an hour ago and breathing the air is enough to become infected.
Incubation is 7-14 days before the prodrome of fever (up to 104 F) and “cold” begin for 2-3 days before sore throat and rash hit. Measles is one of the leading causes of death world wide due to the frequent complications of encephalitis and pneumonia.
It’s a virus, there is no direct treatment only supportive care and oral vitamin A.
The measles vaccine led to a more than 99% reduction in the U.S.—that was until the Andrew Wakefield scam (which lost him his license).
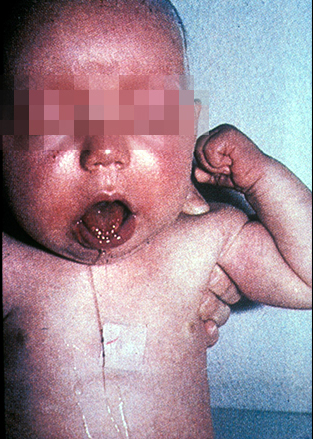
Infectious Parotitis (Mumps)

Mumps is a viral infection of the parotid gland at the corner of the jaw and is usually accompanied with a fever and feeling crappy. Pain actually gets worse with anything that calls for salivation so getting a sick child to eat or drink is very difficult.
Because it’s a virus, there is no specific treatment except supportive care and keeping your fingers crossed that it does not progress into any secondary illnesses like meningitis, deafness or sterility. Half of children with mumps, we’ve recently found, actually DO develop meningitis but at a mild asymptomatic level—except the few who progress to a deeper level.
By the way, the “crazy’s” on the internet who claim the immunizations don’t work may be deliberately using the cases of parotitis caused by enteroviruses in order to trick you into believing them. The other causes of the disease are NOT as contagious, debilitating or damaging to the nervous system.
Erythema Infectiosum (Fifth Disease)

For the most part, infection with parvovirus V19 (Fifth Disease) is generally a mild, self-limited illness (fever, headache, runny nose) and sometimes even asymptomatic.
In a few days of the infection most develop a “slapped cheek” facial rash which, on occasion, progresses to a generalized, pruritic rash.
Like measles, it easily spreads through respiratory secretions when a person coughs or sneezes and is very contagious.
Such a common and mild disease you would think would be with little consequences, and it mostly is, except to pregnant women where it can cause hydrops and fetal death and others who have blood problems like sickle cell disease, hemoglobinopathies and immune-deficiencies.
Impetigo contagiosa

This rash you see on children in grocery stores, malls, classrooms… about everywhere, especially in rural areas. It’s the most common skin infection in children accounting for at least 10% of all skin problems in pediatric clinics.
Just about anywhere that suffers trauma or abrasion (i.e. lips, around nose, knees etc) can become infected with group A strep, staphylococcus or both together and begin to weep and crust into the surrounding skin. It is a common secondary infection of chicken pox lesions.
Without treatment it seems to go on forever and most importantly is highly contagious to anyone coming in contact with a cut, abrasion or sore.
Treatment is with topical or sometimes even oral antibiotics, local wound and supportive care.
Prevention of spread is with careful hygiene and washing, appropriate bandaging and careful washing of touched items.
Scabies

Scabies is also common in children and is contagious by direct contact with an infected person. It is a tiny arthropod, Sarcoptes scabiei, which causes all the itching and rash.
In older children and adults it is most often seen in the webbing of the hands but younger children often are inflicted on their arms, legs and trunk as well.
The mites burrow into the upper layer of skin to lay their eggs with produces intense itching. Diagnosis is made by scraping the rash and burrows and finding either mites, mite feces or eggs under the microscope.
Messing with over-the-counter salves, ointments and home remedies just wastes time and give the “beasts” time to create more extensive and difficult to treat tunnels. Prescription topical scabicides and supportive care are the only way to go—with these additional instructions to prevent RE-infection:
“All family members and close contacts should be treated, even if they are asymptomatic, to prevent reinfection. All bed linen and clothing should be washed to remove eggs and mites. Fomites can persist for 2-3 days without a host. Articles that cannot be washed should be kept in sealable plastic bags for 3 days.”
Pertussis (Whooping Cough)
I actually was expecting by now to no longer consider whooping cough on this list of back to school diseases parents and teachers need to watch out for. Alas, however, it’s still out there thanks to the drop in immunization rates.
We don’t include the many, many respiratory illnesses which everyone knows inhabit all the confined spaces children congregate; but, whooping cough is so hurtful to not only the infected child but all those in the community around them it must be counted on the list.
It is highly contagious through respiratory secretions. Symptoms develop anywhere between 7-10 days to 6 weeks! Usually starts with a mild cough, runny nose and fever for 1-2 weeks; then progresses into SEVERE spasms of coughing followed by a “whooping” sound gasping for air and often vomiting.
These symptoms can last more than 10 weeks!
So far, the bacteria responds to antibiotic therapy which must begin early to ameliorate the signs/symptoms and prevent transmission to others.
Meningococcal meningitis
I have a bone to pick with this organism as I revealed previously. I vowed that it wouldn’t get a chance to catch me off-guard again and (so far) it hasn’t. And now we even have an immunization against it.
The “Neisseria” class of bugs aren’t all as evil as this one but the “meningitidis” is just plain hateful—it causes meningitis and death; but, is deceptive, stealthy and explosive in the way it goes about its business—just like a rattle snake.
Like the snake, on occasion (but not always), it sends out a warning that is easy to miss. The kind of rash it creates is different. A tiny blood vessel ruptures to form a hemorrhage the size of a splinter (petechiae).

A child may develop one or a few tiny petechiae anywhere, easily interpreted as a bruise; and then, within hours or minutes, look like the photo on the left or even the photo on the right.
A person is infected via respiratory droplets in the air, often from a totally asymptomatic carrier of the disease. From exposure to a full brain infection can take less than three days but up to seven.
Often the child appears more ill than you can find reason for, even on a thorough exam. There may be fever, malaise, headache, nausea, vomiting; when it progresses to stiff neck, sensitivity to light and altered mental status it means blood vessels are becoming involved.
Meningococcal meningitis is: a medical emergency, treated with antibiotics, fatal in 50% of untreated cases, leaves most survivors with disabilities including loss of limbs and fatal 5-10% of the time even with prompt treatment… BUT, now has three types of immunizations available to prevent it!
Strep Throat (GABHS)
We’ve already mentioned strep throat above when we talked about scarlet fever. However, next to “colds,” strep throat is probably the most common ailment school children contract so probably deserves mention on its own.
It respects no age limit but for some reason children between 5 and 15 have the lion’s share of GABHS which often comes on sudden 2-5 days after exposure to nasal secretions or saliva from an infected person.

Symptoms may be mild or severe, usually with fever and edema of tissues in the throat. Sometimes there is pus on the tonsils, if they still have them and possibly small red dots on the upper soft tissues.
Doctor’s used to think they could tell whether the sore throat was strep or not by examining the throat; studies, however, have proven that is not the case because other things cause the same symptoms and sometimes strep produces little or no symptoms—which makes the person a “carrier.”
We have TWO tests for diagnosis: the “real” culture and the “quick” test. Here’s the thing though: the quick test is 99% specific so if it’s positive there IS strep; however, it’s sensitivity isn’t great so misses 30%. That means a doctor should do a “real” culture when the quick test is negative.
But remember our concern for strep in children 2 years and older who can develop rheumatic fever if they don’t receive full antibiotic treatment within 9 days of positive confirmation of the infection.
Influenza
Do a search for previous articles on the subject to remember: the confusion often seen with the term “flu,” the description of the disease in children and that viruses can only be prevented (through immunization) and not treated with antibiotics.
Influenza is highly contagious by surfaces and respiratory droplets and seems to “morph” a little from year to year making prevention difficult.
The best way to prevent the disease is by getting a flu immunization each year beginning at 6 months of age and every September or October thereafter.
One new thing we’ve just learned is that our attempt to make the things a bit easier for children by using a nasal spray doesn’t really work well. It was withdrawn from the recommended schedule beginning in 2016.
5 Posts in Back 2 School (back2school) Series
- Refresh: 15 Back to school diseases – 16 Oct 2017
- 5 Back 2 School Issues – 26 Aug 2014
- Back 2 School 2: Mumps - Flu – 4 Oct 2013
- Back 2 School 1: Tinea - Measles – 28 Sep 2013
- Back to School: Intro/Index – 26 Sep 2013
Advertisement by Google
(sorry, only few pages have ads)

