Pediatric Brain Injury – Improved Outcome With Early Nutrition
Ok, this is technically just bizarre and I’m not sure how to really present it; BUT, this issue about brain injury is just so compelling and important (if it’s true) that it clearly must not go unsaid.
The bizarreness comes because a “back-door” finding in a “brain injury and hypothermia” study showed a substantial finding about an “un-related” issue: feeding!
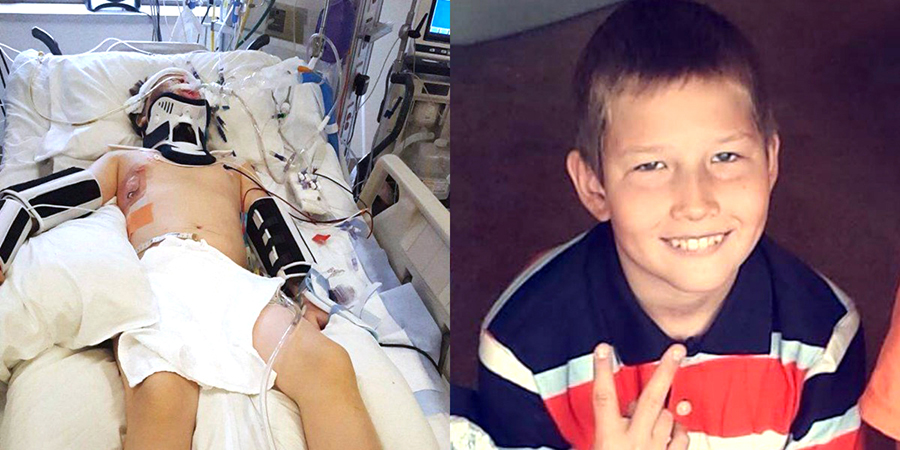
Skateboard neck and head injury for sure
I’m sure you’ve heard about the miracles which happen when children are found drowned in ice water and then are resuscitated when rewarmed.
Well, researchers wanted to know if there, just perchance, also might be some protection given to the brain given by cooling the body when people have head injuries.
A study was designed to discover just that – even had a cool name and everything: “the Cool Kids Trial”.
However, when they were half-way through (77 kids) they tested the statistics a little and found that there was absolutely no benefit showing up in spite of very extensive, time consuming and risky extra procedures; so, they abandoned the study [Lancet Neurol. 2013;12:546-553].
Brain Injury – Nutrition
Surprisingly, in sort of a “lemon into lemonade” move, other researchers moved on to noticing another phenomenon uncovered in the study and reported about it instead: “‘feeding’ comatose patients helps them heal!”
No duh! That was their big insight.
BUT, in fairness, this is kind of a big deal to have in writing! Especially to me.
Brain Injury and Nutrition
You see, one of the very first times I can remember being “belittled” or embarrassed during my medical training was over merely asking the question of an attending in grand-rounds about when we should start considering parenteral alimentation (nutrition via IV solution) in a child who had been comatose for almost a week. His smart-#$$ reply was a condescending: “you worry about saving his life first and then about feeding him.”
Looking back, I can see that my question had completely caught him off-guard and he considered it a slight to his management of the patient. But, the thing was, the entire pediatric medical staff was there, heard the question plus his flippant retort and blankly stood there giving assent by not offering a contrasting opinion.
Now days, even before THIS study, we are a WHOLE LOT less cavalier about nutrition in the healing process. With 40-years worth of retrospect, it was not my question which was foolish (or me for wondering about it). I was spot-on and he should have been embarrassed that he had not considered it by that point – just sayin’.
“Cool Kids” Brain Injury Study
This is what they were going to do: After a lot of previous work to make sure it could be done and was predictably safe they registered with the government clinical trials system [NCT00222742] so patients could be included from many hospitals and countries. They only took children under 18 years of age who were in a coma due to head trauma and who could be cooled down within six hours.
Their computer randomly assigned patients to “normal temperature” treatment (standard) or hypothermia treatment (89.6-91.4 °F); all other standard coma protocols were identical. The research group children were re-warmed after 2 to 3 days. If they survived the Traumatic Brain Injury (TBI), outcomes and functioning were assessed at 3 months for comparison by researchers who were “blinded” to the patients outcome.
This is what they actually found: Unfortunately, after 77 children had been entered into the study, the “take a peek” statistics showed absolutely no difference so the study was terminated for futility.
Just so you can have an idea of the seriousness of the issue, about 13% of the children in the study (both groups) died before the 3 month assessment.
“Cool Kids” Brain Injury “Nutrition” Study
Fortunately, as is the case in most research, they collected more data on each patient than was completely relevant to the hypothermia aspect of the study. This included the hospital record which contained information about nutrition – you know, what, when and how they fed the kids.
Even though everyone on the planet should know that nutrition is important for growth and healing, what they found was that actual nutritional support for the brain injured children varied all over the place. Slightly over a third (35.5%) of the children got nutrition under 48 hours after their head injury.
An additional 40% percent received nutritional support between 48 and 72 hours after they were injured. Nineteen percent more received it more than 72 hours afterward and almost six percent (5.6%) got no nutritional support during their study period.
The researchers found that: the mortality rate was statistically, significantly higher in the children who did not receive nutritional support during the study period; and outcomes (Glasgow Outcome Scales) were significantly worse (both at P < 0.05).
Their conclusions: “Initiation of nutritional support early after TBI was associated with decreased mortality and increased favorable outcomes.”
What Does This Mean For Hurt Kids and Parents?
Despite the fact that in the U.S. Traumatic Brain Injury is responsible for 1.4 Million US hospital visits, 275,000 hospitalizations, 52,000 deaths and more than $56 Billion in costs every year, there still remains an embarrassingly large number of questions about medical care that don’t have good answers! And most everything about nutrition is in that category.
TBI is the leading killer of children over the age of 1 year – accounting for 7440 yearly deaths in the most recent data from the CDC – and close to 125,000 children are currently living with a TBI-related disability. Still, our understanding of how to care for children with TBI is rudimentary.
Studies like these, as limited as they are, are VERY hard to come by because the stakes are so high for “experimenting” with kids – even when “normal” treatment is so vague.
What can you do? Make every effort to obtain care at a pediatric trauma center (even if transfer is needed) who will follow the most recent protocols AND don’t be afraid to talk with your physician about things like nutrition. It’s not a dumb question!
“Nutrition Allows Healing”
[Society of Critical Care Medicine’s (SCCM) 45th Critical Care Congress: Abstract 17. Presented February 21, 2016]
11 Posts in Childhood Concussion (concussion) Series
- Helmits?! Do they prevent concussions? – 5 Apr 2017
- Video- concussion management – 30 May 2016
- Video: Concussion 101 – 6 May 2016
- TBI, concussion and early nutrition – 28 Apr 2016
- 5 things to know – 12 Sep 2015
- Football and brain damage – 21 Aug 2015
- 10 scary issues – 18 Jun 2015
- Reading test a predictor of concussion – 30 May 2014
- New guidelines for sports – 27 Jul 2013
- More dangerous than we thought – 24 Jul 2013
- Childhood Concussion Series: Intro/Index – 23 Jul 2013
Advertisement by Google
(sorry, only few pages have ads)