Otitis Externa: Swimmer’s Ear, More Than An Annoyance
“That gunky, smelly, puss draining out of your son’s ear is an infection called ‘Otitis Externa‘ – or possibly Otitis Media that has ruptured and is draining.
With the history you gave I’m guessing it’s ‘externa’ – you can call it ‘Swimmer’s Ear‘ but I don’t, cause it’s certainly caused by a lot more things than merely swimming.”
An eleven-year-old’s draining ear due to otitis externa
Otitis Externa (Swimmer’s Ear)
In medical parlance, “Otitis” means “ear infection” – an “itis” of the ear; and “externa” is Latin for “outside – or in this case outside the eardrum in the canal or the floppy part on the side of your head (auricle) – hence: Otitis Externa (OE).
The reason we have skin (according to Milton Burl) is to keep our insides from falling out; AND, (according to me) to keep the ‘bugs’ out – which it does rather effectively unless something causes the skin to weaken or break.
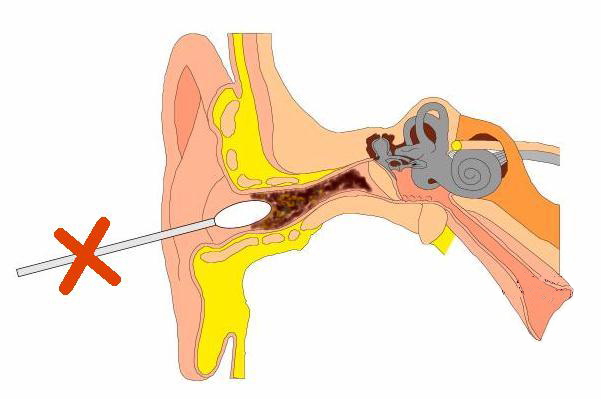
A scratch or scrape (like sticking something in your ear to scratch or remove something) or merely water-logging it can allow any bacteria in the canal or water to schlep inside and set up housekeeping. Some bacteria are better at it than others and it usually is a bacteria.
An issue is that, although the auricle doesn’t feel unusually sensitive to pain compared with other areas, the skin inside the canal is terribly sensitive and OE is nearly always painful.
In developed countries, where medical care and health departments are readily accessible, OE rarely causes serious problems or issues; however, if it is left untreated or is treated poorly (like much of the info on the internet) it definitely can cause significant issues as the infection attacks deeper tissues progressing to bone infection, deafness and loss of tissue.
Prompt diagnosis is highly important in patients who are diabetic or immunocompromised in some way because it can develop into necrotizing (malignant) OE, a potentially life-threatening infection.
The lion’s share of OE cases are “Acute diffuse OE” over the chronic, localized or eczematous types; and, OK, it typically is seen in swimmers and nearly always on one side only.
OE Symptoms and diagnosis

Onset of symptoms is usually within 48 hours (considered fairly rapid) and they are basically those of external auditory canal inflammation – ie pain, itching, ringing, hearing loss and fullness with or without jaw pain.
Of course we’ve mentioned otorrhea (draining) already but there can also be signs of infection outside the canal like swollen glands and tissue swelling or redness of the outside ear.
There is usually a history of an activity in water and often a history of preceding trauma, like forceful ear cleaning, use of cotton swabs or water in the canal.
An exam trick we use in diagnosing OE is to gently press on the Tragus (the little pointy thing in front of the ear canal) which transmits the movement to inside the canal and makes the pain worse.
Of the ninety or so percent of OEs that are caused by bacteria, the majority of them are due to a Pseudomonas species but Staphylococcus, anaerobes and gram-negative organisms all do their share.
Usually a doctor can make the diagnosis by examination alone and no tests are needed. The color and smell and ear exam are enough and treatment is usually begun “empirically” or what we call by presumptive diagnosis alone. [On the other hand adults with an OE should get a test for diabetes]
However, that means that even though the majority of children get treated earlier and less expensively, there are occasional children who don’t initially respond so need cultures, different antibiotics and perhaps a referral to an ear specialist.
If the OE develops complications, it will naturally require deeper testing such as x-rays, CT scans or even MRI and bone scans.
Treatment

Although it’s tempting for a doctor to prescribe both an oral antibiotic AND antibiotic ear drops, we now know that the lion’s share of children with OE respond to ear-drops alone.
Oral antibiotics are generally reserved for patients with fever or other complications like: immunosuppression, diabetes, adenopathy, or an infection extending outside of the ear canal. Inflammation into the face or neck is more severe and needs antibiotics taken internally in order to heal, and sometimes when the canal is so swollen that drops won’t penetrate we use pills then too.
There are some drops that are much more expensive (and not reimbursed by all insurances) but less expensive medicines are very reasonable treatments too (i.e. Cortisporin Otic – in U.S.). If there is a possibility that the eardrum might be perforated we may need to use alternative drops.
Risk Factors for OE
Besides swimming there are other risk factors too. For example if there is little or no cerumen (wax) the skin will become dry and crack – an easy access for bacteria. It also itches and predisposes to mechanical devices to scratch, which can injure the skin and cause infection.
High humidity and increased temperature is, of course, a factor as is local trauma – like from cotton-tipped swabs; and ear-piercings, they dispose to infections too.
Blockages like from wearing hearing aids, blue-tooth telephone devices and headphones produce a lot of OE infections; and, believe it or not, exposure to cold water (like in surfers) creates bony “bumps” in the ear canals called exostosis which can do the same thing.
Lastly, some children are just born with narrow, curved or “windy” ear canals which are hard to drain of liquid and therefor cause pooling and excess moisture that infections love to get started in.
Other Causes of OE
- Acute Diffuse OE: This is the most common type of OE – the kind we often see in swimmers
- Acute Localized OE: Also known as furunculosis, this type of OE is associated with an infected hair follicle
- Chronic OE: This infection starts out like ordinary OE but lasts for longer than 6 weeks and needs several courses of alternate antibiotics along with other measures like cleaning and drainage.
- Eczematous OE: This type is related to atopic dermatis, usually manifesting on other areas as well – psoriasis, eczema and other conditions.
- Necrotizing “malignant” OE: This occurs when the inflammation extends into deeper tissue outside of the auditory canal and is often secondary to the patient being immunocompromised in some other way like with diabetes, AIDS or cancer. The infection may be in the skin (cellulitis) or even the bone (osteomyelitis).
Ear Wax
Many parents seem to have a preoccupation with ear wax, cerumen we call it! Not the kids, they don’t want anything inside their ears (believe me I know); but, the internet is bursting with postings by people with ear fetishes (or profit motives) trying to get you to rinse, flush, Q-tip and candle the stuff out of your ears.
Don’t give in to the foolishness, cerumen is a healthy defense for the external auditory canal. Besides keeping the skin soft and flexible, it’s generally acidic (pH 4-5) which inhibits both bacteria and fungi.
Swimmer’s ear develops in swimmers because of excessive water exposure – which reduces cerumen and creates dryness and itching in the canal. That’s when “something’s gotta scratch that itch” and you’re tempted to reach for the Q-tips, pencils, paper-clips, anything handy.
Nine Things To Remember In Treating Otitis Externa – Swimmer’s Ear
- No swimming! Swimming is not allowed until the infection is completely cleared, usually 10 days to 2 weeks, not only for the patients benefit; but, all that pus and bacteria shouldn’t be spread around in pools for others to swim in!
- Analgesics: There is no question that the ear canal is one tender place and can produce an inordinate amount of pain. For normal cases, especially in children, aspirin or acetaminophen is often all that is required. For moderate or severe cases 1-3 days worth of “stronger stuff” may be used. Things should be dramatically improved by the 72 hour recheck visit – usually when it’s done.
- Water protection: We’ve already said no swimming so what else could there be? Well, the ear needs to be kept dry during showers, shampoos, etc. which can be done by applying petroleum jelly to a cotton ball and gently placing it in the ear.
- Warm compresses: If needed for pain, a heating pad or warm towel can be placed over the area for 10-15 minutes, 3 times daily.
- A soft diet: Sometimes chewing is painful so a soft diet might be helpful in minimizing the pain of jaw movement
- Don’t put anything in the ear: Hearing aids, earplugs, headphones or blue-tooth ear phones should not be inserted until the infection clears.
- Use Medicated Ear Drops Correctly: To work they must penetrate into the ear canal. Lie down with canal upward to place drops and remain that way for a minute or so. Sitting up the drops should NOT run back out. And use for the full prescribed course NOT just until the pain is gone. Remember it’s the infection that needs killing not just the pain.
- Watch for Complications: You can tell if things aren’t improving like they should be within 24 hours of beginning medication. Also watch for spreading into surrounding tissues.
- Prevent Recurrence: Those prone to recurrent OE should ascertain thorough drying of the ears (without Q-tips) using a hair-dryer set on low and held enough away so not to cause burns, if needed. A custom mold can be made which prevents water from entering the ear during swimming if recurrences are a problem.
Advertisement by Google
(sorry, only few pages have ads)

