New Emergency Measles Guidelines
I really hope that by now you’re getting the idea that everyone who truly understands the problem is scrambling around trying to plug the dike on “this measles thing.” The American Academy of Pediatrics (the US organization most charged with advocating for children’s health) is even making available to the public the chapter on measles guidelines months before the full book was set for its normal publishing. And for Free – believe it or not!
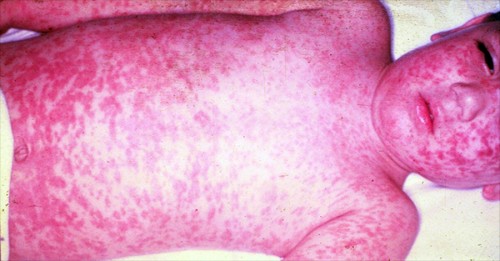
Toddler in hospital severely ill with measles
The “Red Book” is regularly published to physicians and contains all the updated information on infectious diseases they need to know. Now, before even the typography is completed, the new information on Measles is felt to be so important to controlling the current measles epidemic that their ‘draft’ is being made available.
Measles Guideline Changes 2015
I’ll highlight some of the more salient features here but feel free to use the above link to read the whole article. Notable changes from previous guidelines are in the areas of: the evidence required for measles immunity, the use of immune globulin, vaccination for healthcare personnel, and the management of patients with HIV infections and other susceptibilities.
Evidence of Immunity
Now that the politicians have gotten into this, there is NOTHING LIKE TAKING YOUR WORD for it anymore. You’ve got to have an official document giving the specifics of the immunizations your children have received when meeting any legal requirements for school/work entrance or travel.
That means that your current doctor (who is filling out the forms) must also be able to verify specific dates and places from your, or any previous providers, records or it doesn’t meet the “evidence of immunity” and he/she must take measures to either ascertain immunity by blood work or re-immunize – which is cheaper and usually the way to go.
Evidence of immunity to measles includes any of the following:
- Documentation of age-appropriate vaccination with a live measles virus-containing vaccine:
- preschool-aged children: 1 dose;
- school-aged children (grades K-12): 2 doses;
- Laboratory evidence of immunity;
- Laboratory confirmation of disease;
- Born before 1957*
Use of Immune Globulin
Immune Globulin is when they extract the “immunoglobulin” (part of your blood that makes you immune after a disease) from someone who has already had the measles, put it into a serum and inject it into someone who needs it for some reason.
Your doctor can administer it either intramuscularly or intravenously within 6 days of exposure to someone with measles in order to prevent (possibly) or modify (more likely) the case of measles you’re likely to get. Obviously it’s used in people who lack evidence of measles immunity.
The usual recommended dose is 0.50 mL/kg administered intramuscularly (maximum volume of 15 mL); however, those who are at higher risk for complications from severe measles should receive intravenous application at a dose of 400 mg/kg.
Once a child or member of the family has received Immune Globulin it definitely disrupts normally scheduled immunizations and there is a long list of “what if” scenarios that your doctor will need to consider in order to get back on track.
Vaccination of Healthcare Personnel
This one is as easy as it is obvious: All healthcare entities should have set policies and programs to ascertain complete and up-to-date immunizations of all personnel, including students, who may be in contact with patients who might have, or been exposed to, measles – or with other employees who are in contact with them.
Guidelines warn that “birth before 1957 (when immunization programs were invented) is not a guarantee of measles immunity” and that facilities should “consider” vaccination of unimmunized healthcare personnel who lack laboratory evidence of immunity even though they were born before that year.
HIV and Other Susceptibilities
There is a growing number of children who are being treated for HIV. As you can imagine, there are also equally large numbers of complicating factors that need to be considered if a severely immunocompromised child is exposed to the Measles virus.
All the ramifications can’t be discussed in an article like this, the child’s physician will figure it out; BUT, I mention it here to provide perspective about WHY MASS COOPERATION WITH IMMUNIZATION PROGRAMS IS NECESSARY.
The only hope for safety that these sick children (or infants) have is when the Measles virus no longer is being ubiquitously spread around the population – and long experience with this virulent virus has shown us that only occurs when there is less than 3% of the population running around without immunity!
Physicians managing immunosuppressed or compromised patients should have ready record of the child’s immunity status. They need to make sure that the child gets their MMR shot BEFORE giving other medicines which might interfere with the child’s response to the immunization. They need to watch against giving live-virus vaccines to immunocompromised patients and they need to avoid immunizations for at least a month in diseases which has required corticosteroids.
There is a lot to consider now that this “Chamber of Secrets” has been re-opened. If you’ve still got any questions feel free to comment or contact or read the full text of the new recommendations.
Recommendations for Measles Immunization
As a recap, let’s look at a decision-tree for Measles Immunization in children in different situations.
| Category | Recommendations |
|---|---|
|
Unimmunized, no history of measles (12 through 15 mo of age) |
MMR vaccine is recommended at 12 through 15 mo of age; a second dose is recommended at least 28 days after the first dose and usually is given at 4 through 6 yr of age |
|
Children 6 through 11 mo of age in epidemic situations or before international travel |
Immunize with MMR vaccine, but this dose is not considered a valid part of the immunization schedule, and 2 valid doses administered on or after the first birthday are required. The first valid dose should be administered at 12 through 15 mo of age; the second valid dose is recommended at least 28 days later and usually is given at 4 through 6 yr of age |
|
Students in kindergarten, elementary, middle, and high school who have received 1 dose of measles vaccine at 12 mo of age or older |
Administer the second dose |
|
Students in college and other post-high school institutions who have received 1 dose of measles vaccine at 12 mo of age or older |
Administer the second dose |
|
History of immunization before the first |
Dose not considered valid; immunize (2 doses) |
|
History of receipt of inactivated measles vaccine or unknown type of vaccine, 1963–1967 |
Dose not considered valid; immunize (2 doses) |
|
Further attenuated or unknown vaccine given with IG |
Dose not considered valid; immunize (2 doses) |
|
Allergy to eggs |
Immunize; no reactions likely (see full text for details) |
|
Neomycin allergy, nonanaphylactic |
Immunize; no reactions likely (see full text for details) |
|
Severe hypersensitivity (anaphylaxis) to neomycin or gelatin |
Avoid immunization |
|
Tuberculosis |
Immunize (see full text for details); if patient has |
|
Measles exposure |
Immunize or give IG, depending on circumstances (see full text for details) |
|
HIV infected |
Immunize (2 doses) unless severely immunocompromised |
|
Personal or family history of seizures |
Immunize; advise parents of slightly increased risk of seizures |
|
Immunoglobulin or blood recipient |
Immunize at the appropriate interval (see full text for details) |
[American Academy of Pediatrics. Early Release From Red Book: 2015 Report of the Committee on Infectious Diseases. Full text]