Heat Illness In Children: Heat Stroke, Rash, Exhaustion
With summer comes heat – at least that’s how we do it in the U.S. (so far). And, for most of us: Summer Vacation, Little League and lot’s of sun.
Teen suffering heat stroke after running
We’ve talked about sunburn and its prevention and treatment before. Now lets discuss another group of illnesses which has been given the moniker: “Heat Illness.”
Illnesses Caused By Heat
Several relatively minor (mostly) conditions all have the same root cause and treatment – heat rash, heat cramps, heat syncope, and heat exhaustion. Additionally the more severe condition of heat stroke is included, and we’ll cover all of them.
Just like the environment’s ambient temperature is a compilation of many components, the human body’s response also depends upon multiple factors and develops gradually. It may, however, become obvious suddenly once the body’s several compensating mechanisms begin to fail.
Heat Stroke
We define heat stroke (or sunstroke) as a “body temperature that exceeds 40.5°C (105°F) due to environmental heat exposure with lack of thermoregulation.” The “lack of thermoregulation” (i.e. sweating) is due to either the fact that the body has already tried to compensate and failed, or that it is blocked by other illnesses, conditions, alcohol or some drugs.
Additionally, body size makes a substantial difference and it should be said that a body’s response to heat may progress through the various illnesses depending upon the length and severity of exposure.
A baby bundled with three layers of clothing wouldn’t be able to “thermoregulate” even if he was able to sweat effectively. A runner can no longer cause cooling through sweating when he continues to run and is becoming dehydrated.
Exposure to hot climates without sufficient shade, water, or proper clothing is but one of the areas of risk. Poor hydration because of illness, poor fluid intake, or excess alcohol consumption also increases the risk.
Of course unconditioned, weekend “athletes” engaging in strenuous physical activities are often less prepared and are at especially high risk; but, even seasoned athletes may succumb – especially with extreme sports such as ultramarathons.
Symptoms of heat illness
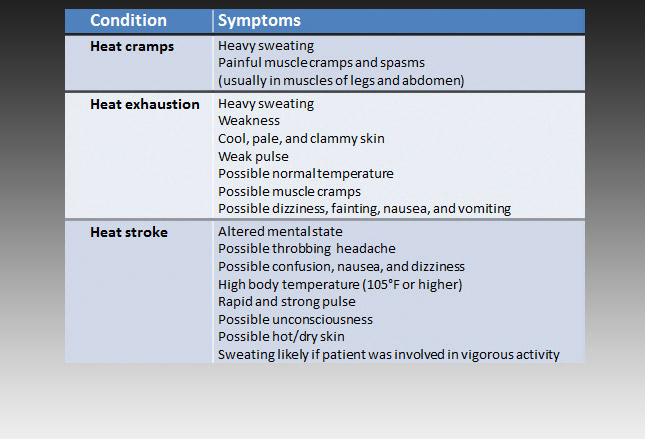
The table (click to enlarge) shows typical symptoms of heat illnesses such as heat: cramps, exhaustion and stroke; and is given in a way to depict the typical “progression” in severity.
For expediency we talk about two forms of heat stroke: Exertional – usually effecting younger people; and nonexertional – usually effecting sedentary, older folks, the chronically ill and the very young.
Exertional heat stroke is from prolonged, strenuous physical activity in a hot environment and nonexertional is usually from unusual environmental heat waves where people aren’t prepared.
Both types of heat stroke are associated with a high morbidity and mortality, especially when therapy is delayed. It causes up to 1,800 deaths in the United States each year with greatest impact in the Northeast and Midwest – where residents are NOT acclimatized (nor expecting) high heat.
Early recognition of symptoms is critical to avoiding deadly neurologic damage, cardiovascular collapse, pulmonary damage, gastrointestinal issues, hepatic and renal failure and rhabdomyolysis (muscle tissue breakdown).
Miliaria (heat rash)
The so-called “heat-rash,” or miliaria, is due to blockage of the sweat ducts resulting in the leakage of sweat into the surrounding epidermis or dermis (skin).
The rash looks like small pimples, which are usually pinkish in color, and is nearly always found on parts of the body covered by clothing. They develop within minutes or hours after the body is triggered to sweat.
They usually resolve in less than an hour after the sweat-inducing stimulus (i.e. heat) is removed. Some individuals are more prone to developing heat rash and they are then usually more prone to developing the next stage: heat exhaustion – due to their inability to sweat efficiently and dissipate heat.
Heat Exhaustion
Some people call heat exhaustion “almost heat stroke.” It is more correctly called “heat exhaustion”; but, it is true that it is “almost heat stroke,” IF the warning signs are not recognized or heeded.
Unfortunately, heat exhaustion is often a precursor of heat stroke. Symptoms include profuse sweating, rapid breathing and a fast, weak pulse. Those are all the symptoms of a person’s body trying desperately to cool itself down before it runs out of enough fluids to sweat.
This is the stage where treatment must begin immediately in order to avoid the tipping-point into “stroke.”
Heat Stroke
Once the body’s compensating mechanisms begin to fail, due to fluid depletion or illness, its core temperature begins to rise above 40.5°C (105°F) and the symptoms listed above for “exhaustion” progress into hot/dry skin, rapid heart rate and vomiting. The skin was wet from perspiration but sweat is becoming “all used up” leaving the skin dry and hot.
The excessive heat actually causes the muscle fibers to begin breaking down into myoglobin which is then excreted in the urine – known as rhabdomyolysis, which can lead to renal failure and coagulopathies (bleeding problems).
As the central nervous system looses its preferential protection from excessive temperatures, symptoms such as confusion, ataxia, seizures, and delirium take over. This is the real deal, is difficult to reverse and often fatal. Even with recovery there is often damage. Did I say “early recognition and treatment” is critical?
Treatment
Everyone thinks of ICE as the treatment for heat stroke; but, the first thing that must happen is to REMOVE the patient from the CAUSE of the heat. Get them out of the heat. If it’s the sun, don’t merely just shade their eyes, get them fully into the shade or air-conditioning.
Secondly, think of fluids, if they are conscious enough to swallow them – as much as they can take and cool is best. And thirdly begin taking steps to cool them down. Preferably do all three at once, or in quick succession.
There are many cooling techniques to use, evaporative cooling is usually the quickest available. Remove all clothing down to the minimum appropriate for the location and pour water on them enough to soak them down. Evaporation should cool core body temperature by 0.3°C per minute if you keep them wet and can keep air circulating.
Transportation to a more secure place for treatment needs to be accomplished. All clothing can be removed and cool mist can be directed on them with a large fan (best) or a wet sheet can be placed over them.
Ice packing is also used both for first aid and full-blown emergency room treatment. Ice in contact with the axillae, neck and groin are the most important areas but the scalp is also important for smaller children and infants.
If the patients condition is severe, ice water immersion can reduce core body temperature by about 0.15°C per minute but is used with caution in the elderly or those with other medical conditions for fear of causing other problems and making their condition worse.
The ER has other techniques to use as well; such as: drugs to prevent the patient from shivering (thereby increasing temperature), intravenous fluids and flooding cool fluids into the stomach, bladder, peritoneum and rectum. In dire cases, where circulation is impaired due to dehydration, fluids can be injected directly into the bones.
The patients temperature must be measured at it’s core (rectally or esophagus) in order to even be close to accurate and it should be taken frequently during treatment to assess/assure progress back to normal. Once core temperature reaches 39°C (102°F) the cooling techniques are discontinued in order to prevent rebound hypothermia (low temperature).
Obviously, aspirin or acetaminophen do NOT work in heat illness. “Last resort” efforts can be used in the hospital such as: hemodialysis, cardiopulmonary bypass and intravascular cooling.
Prevention
I hope I’ve described enough about the full blown disease to convince you that PREVENTION of heat illness is nothing to be taken lightly! There’s nothing “sissy” about a “cool down/hydration” timeout in a game and the water jug can’t be accidentally left at home on the counter. Water must be made available FOR FREE at all gatherings of crowds not only sports events. Doing otherwise is irresponsible.
Athletes need clothing of lightweight, moisture-wicking fabric and freely available water to drink. Sports drinks or energy drinks are really not usually needed BUT coaches must not merely think all they need to do is tell players “be sure and drink.” That often does NOT work because by the time a person becomes thirsty they are already becoming dehydrated!
The point is to DRINK BEFORE YOU GET THIRSTY in order to prevent dehydration. If for no other reason, coaches should make the effort because getting ahead of dehydration improves performance – a whole lot better than a lot of other things we do.
Sports Drinks
Sports drinks are flavored water with variable amounts of carbohydrates, vitamins, minerals, and electrolytes added and are the fastest growing beverage market – children’s sports should almost never require them.
Water is always the preferred beverage for training and even competition sessions at moderate intensity – NO supplements are necessary. With prolonged vigorous activity, simple carbohydrates might help maintain blood glucose as muscle glycogen stores are depleted.
Only with prolonged and intense exercise and very hot/humid conditions might sports drinks become an acceptable choice. Competitions short of some high-school and college events would not be appropriate in children’s sports.
Energy Drinks
Energy drinks are those drinks filled with stimulant substances, like caffeine and guarana. These, to most health professionals and children’s advocated, are NEVER INDICATED in children’s sports – pure and simple. They may contain carbohydrates, vitamins, and minerals but their main benefits are the perceived or real stimulant effects touted in their advertising.
Children, teens and parents often think that the name “Energy” refers to the carbohydrates in the liquid; but, that is NOT TRUE. “Energy Drink” refers to those that contain stimulants, i.e. large amounts of caffeine and often guarana (a stimulant used to increase the caffeine content even more.)
Caffeine only minimally increases endurance and strength BUT has never been studied specifically in children due to the significant side effects – such as increased blood pressure, heart rate AND TEMPERATURE. (It may even put children at even greater risk for heat induced illness!) Additionally, especially in children, it can affect mood and sleep and is associated with increased anxiety and irregular heart rhythms.
Intake of all non-medically indicated stimulants in children is highly discourage at any time let alone in needless so-called “energy drinks.” If the New York mayor wants to ban something appropriate it should be the entire class of “energy drinks.” Completely needless and dangerous.
Recommendations
Regarding fluid supplements the Committee on Nutrition and the Council on Sports Medicine and Fitness makes the following guidelines:
- Educate kids and parents about sports drinks, energy drinks, their uses and dangers.
- Discourage consumption of energy drinks by children and adolescents due to the stimulants in them.
- Discourage routine use of sports drinks as they lead to excessive calorie consumption and possible obesity.
- Promote the appropriate use of sports drinks – namely for rapid ingestion of fluids, carbohydrates, and electrolytes during or after prolonged vigorous exercise.
- Promote water as the preferred beverage for daily activities and regular sports and exercise.
Advertisement by Google
(sorry, only few pages have ads)