Children’s Back To School Medical Problems – Part 2
Children face a number of medical issues when they leave the relative ease of summer in favor of the more crowded environment of school each year. Here is part two of a list of common illnesses and issues facing us at “back to school” time.
Remember, “Praemonitus, praemunitus” – “forewarned is forearmed.”
Back to School Medical Problems
Let’s see, we’ve already covered head lice; ringworm; hand, foot and mouth disease; scarlet fever; pink-eye; chicken pox; and, measles (Rubeola). You might think that there couldn’t be anything left to cover; ahh, but you’d be wrong. Are you ready to continue testing your knowledge?
Facial Swelling and Fever
 This first grader only got a couple weeks into his schooling life before he developed a fever, felt tired and listless, got a headache and his face and neck began swelling. He had difficulty even swallowing his own saliva.
This first grader only got a couple weeks into his schooling life before he developed a fever, felt tired and listless, got a headache and his face and neck began swelling. He had difficulty even swallowing his own saliva.
This is the Mumps and do you know the treatment? There is none – which makes it fortunate that the disease has become rare in the US because of vaccination programs.
Parotid glands swell and are very uncomfortable but the other complications like meningitis, encephalitis, hearing loss and sterility are rare.
“Slapped Cheek” Rash
 This boy woke up the morning of his ninth birthday party with a rash on both cheeks. In the bath his mother noticed that the warm water seemed to “bring out” the rash on his body as well. She called the doctor who suspected what disease do you think?
This boy woke up the morning of his ninth birthday party with a rash on both cheeks. In the bath his mother noticed that the warm water seemed to “bring out” the rash on his body as well. She called the doctor who suspected what disease do you think?
Fifth Disease (erythema infectiosum), unlike the other five, is a disease which still goes by it’s number from back when doctors could number the childhood rashes one to six. And this was number five.
Compared with the other five, this one is a comparatively mild illness which we now know is caused by parvovirus B19 and which almost always produces a “slapped cheek” rash.
It starts with cold-like symptoms of fever, headache and runny nose; then, after a few days, produces the characteristic rash on the cheeks progressing to the body.
 Children may get sick anywhere from 4 days to 2 weeks after being exposed and infected. The unfortunate part is that 20% of the kids who are infected never develop symptoms themselves but can still infect others.
Children may get sick anywhere from 4 days to 2 weeks after being exposed and infected. The unfortunate part is that 20% of the kids who are infected never develop symptoms themselves but can still infect others.
The disease spreads through the common cough or sneeze of secretions but its complications are not so common – it has a habit of shutting off the body’s production of red blood cells for three or four days. Most normal people who only turn over about 1 percent of their cells a day can handle a 4 to 5% loss without even noticing it.
However, those with diseases like sickle cell anemia, thalassemia or pregnant women who can turn over 10% per day may be in real trouble with 40 – 50 percent loss. So definitely inform pregnant teachers about the risk from exposure.
Weeping, Scabby Rash
 We seem to be on a roll so let me give you another extremely contagious disease. These two boys have the same problem: a weeping, scabbing rash which doesn’t seem to go away. What is the problem?
We seem to be on a roll so let me give you another extremely contagious disease. These two boys have the same problem: a weeping, scabbing rash which doesn’t seem to go away. What is the problem?
Impetigo (impetigo contagiosa) is caused by a couple of bacteria which seem to have developed particular skill in turning any break in the skin into a weeping, crusting sore.
Being highly contagious it is the most common skin infection in children and accounts for 10% of all clinic visits for skin problems in pediatrics.
 It is caused by the bacteria known as “Staph Aureus,” “Group A Strep” OR both – either concurrently or sequentially. Anywhere the superficial epidermis is even slightly broken by a bite, cut, abrasion, trauma – or even another rash, like Chicken Pox! (That’s why we don’t “scratch the pox”).
It is caused by the bacteria known as “Staph Aureus,” “Group A Strep” OR both – either concurrently or sequentially. Anywhere the superficial epidermis is even slightly broken by a bite, cut, abrasion, trauma – or even another rash, like Chicken Pox! (That’s why we don’t “scratch the pox”).
The skin becomes reddened and inflamed, just like most sores, and parents usually treat it with anti-bacterial salves and wait for it to heal normally, like most sores. But, it doesn’t.
In fact, that’s one of the ways you can tell it’s Impetigo – it doesn’t heal normally. It almost always requires a prescription oral antibiotic for it to heal.
An Itch With A Rash
 This boy began sleeping fitfully and became very fussy. His mother noticed him wiggling like he was trying to scratch his back and found this rash when she removed his clothes. What is causing it?
This boy began sleeping fitfully and became very fussy. His mother noticed him wiggling like he was trying to scratch his back and found this rash when she removed his clothes. What is causing it?
Scabies is so intensely itchy that it’s almost like having an “itch with a rash” instead of the other way around. AND, the bug is extremely contagious.
When I say “bug” I mean real bug, animal (well arthropod) not bacteria. Sarcoptes scabiei (sar-kop-tee’s skay-bee-eye) is contracted by direct human contact, including sexual. However, because the things can live without eating for up to two weeks, transmission by clothing, linens and rugs is also possible.
 The little beasties burrow into skin and set up an itch that lives up to its colloquial name: “The Seven Year Itch.”
The little beasties burrow into skin and set up an itch that lives up to its colloquial name: “The Seven Year Itch.”
There is a lotion for treatment BUT all family members and close contacts must be treated in order to eradicate the thing, even if asymptomatic. Every inch of external skin must be covered with the lotion, bar none. Following closely the directions for the brand of medicine you use, if you wash your hands after applying the lotion you need to apply it to them again. Missing even one area is like not treating anything at all.
And that’s just the beginning, all bed linen and clothing should be washed in order to remove eggs and mites. Rugs need to be vacuumed heavily and/or run through the dryer on hot for 30 minutes. Articles that cannot be washed should be kept in sealable plastic bags for at least a week.
After all that, and even if all the bugs are killed, the itch still remains for an extended time while the body removes the bug bodies in the burrows which can’t be washed off.
There IS hope, just not very quick.
The Worst Cough You Ever Had
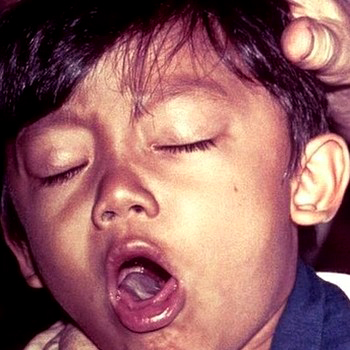 This seven-year-old returned from a visit to Bolivia with a “cold” that seemed to have gotten worse on the plane-ride home. His parents didn’t believe in immunizations so he hadn’t had his first course of vaccines until shortly before leaving for their trip.
This seven-year-old returned from a visit to Bolivia with a “cold” that seemed to have gotten worse on the plane-ride home. His parents didn’t believe in immunizations so he hadn’t had his first course of vaccines until shortly before leaving for their trip.
His low-grade fever hung on and his cough seemed to be getting worse so he was seen in the after-hours emergency clinic – where the doctor recognized the characteristic sound of the cough and admitted him to an isolation ward of the hospital. What disease did the doctor diagnose even before looking at the patient?
Pertussis (whooping cough) got it’s common name from the actual sound children made when coughing until many, if not most, of them died. “cough, cough, cough, cough, cough, cough, cough, whoop.” The final whoop being when the person was finally able to frantically gasp for air.
 Pertussis is caused by Bordetella Pertussis, about as contagious a bacteria as can possibly be, and has largely been eradicated in all developed countries thanks to immunization programs. After breathing in bacteria from an infected persons cough or sneeze, it can take anywhere from 1 to 6 weeks for a runny nose, mild cough and low-grade fever to develop.
Pertussis is caused by Bordetella Pertussis, about as contagious a bacteria as can possibly be, and has largely been eradicated in all developed countries thanks to immunization programs. After breathing in bacteria from an infected persons cough or sneeze, it can take anywhere from 1 to 6 weeks for a runny nose, mild cough and low-grade fever to develop.
That’s when the cough becomes about as bad as a child can stand and still live and lasts for around two MONTHS – which is why many children don’t.
In my years of practice I’ve run across only two parenting issues which seem to be entirely unique to completely “developed” countries: picky eaters and people who say they don’t believe in vaccinations. Only in, for example, the US is food so ubiquitous that a parent can enable such non-life-sustainable habits.
Ana it’s only in the developed countries where parents can rely on the hundreds of other parents who DO believe in immunizations to protect them from the child-killers of former years– “herd immunity,” where “immune” children form a protective barrier around the un-immunized. Leave that barrier and you have no protection.
Fever, Headache and Stiff Neck
 This boy was actually still well when his mother brought him into the doctor to look at a rash of a kind that she hadn’t seen before so was worried. He had a temperature of 100 degrees orally, but otherwise felt fine. His doctor admitted him to the hospital – what on earth do you think for?
This boy was actually still well when his mother brought him into the doctor to look at a rash of a kind that she hadn’t seen before so was worried. He had a temperature of 100 degrees orally, but otherwise felt fine. His doctor admitted him to the hospital – what on earth do you think for?
The rash was a petechia – a tiny, broken capillary under the skin sometimes seen with bumps or when a child has cried strongly. But, they also can be seen in some blood disorders and in some infections, notably: Meningococcal meningitis.
There are many “kinds” of meningitis but the one caused by the bacteria Neisseria meningitides is particularly worrisome with distressing side-effects. The bugs travel on respiratory droplets from person to person, frequently from someone who is basically without symptoms.
It develops within 3-7 days, often with minimal symptoms for a short time, then suddenly the child becomes very ill with lethargy, fever, headache, nausea and vomiting. When the disease is well underway there is a stiff neck, sensitivity to light and altered mental state.
With prompt treatment, the mortality rate is still 5%-10%; without prompt treatment over 50% of children die.
Sore Throat
 This youngster awoke with a fever and very sore throat. His sister had been ill last week and his friend the week before that. The nurse did a quick throat swab which came back “positive” for what?
This youngster awoke with a fever and very sore throat. His sister had been ill last week and his friend the week before that. The nurse did a quick throat swab which came back “positive” for what?
Sore throats are, more often than not, caused by those virus things for which there is no treatment except time and liquids. On occasion however, they can be caused by Group A beta-hemolytic Streptococci (GABHS) which makes them a strep throat.
Commonly children 5 to 15 years develop symptoms 2- 5 days after they come in contact with nasal secretions or saliva from another ill person. Symptoms usually begin suddenly including sore throat, fever, red throat (sometimes with pus), nausea, and tiredness.
Some doctors used to think they were pretty good at diagnosing between strep and non-strep throats because of how red, or amount of exudate or tiny red hemorrhages; but, study’s prove they can’t. And that’s a major concern because untreated strep in children aged 2 years or older can subsequently cause rheumatic fever.
To prevent it, antibiotics should be started within 9 days of infection. We now have rapid antigen detection tests for GABHS are diagnostic if positive because they rarely show false positives (specificity); however, they can miss up to 30% of cases (sensitivity). Therefore, follow-up cultures are necessary for negative results.
Flu Vaccination
 This last medical consideration for when children go back to school is the yearly flu vaccination. There are intra-nasal vaccinations available which some school districts use in a school-wide program to prevent the seasonal illness.
This last medical consideration for when children go back to school is the yearly flu vaccination. There are intra-nasal vaccinations available which some school districts use in a school-wide program to prevent the seasonal illness.
Transmission of influenza is person to person on respiratory droplets and can be spread to others up to about 6 feet away, even after the sick person has left the room! Symptoms begin within 1-4 days after infection suddenly, with fevers, cough, sore throat, myalgia, headache, and malaise.
Vomiting and diarrhea are also often present in children but this is NOT the same as what is called the “stomach flu.” Recovery can be delayed by the development of complications such as bronchitis, pneumonia, otitis media, and sinusitis. The best way to prevent influenza is by getting a flu vaccine each year.
5 Posts in Back 2 School (back2school) Series
- Refresh: 15 Back to school diseases – 16 Oct 2017
- 5 Back 2 School Issues – 26 Aug 2014
- Back 2 School 2: Mumps - Flu – 4 Oct 2013
- Back 2 School 1: Tinea - Measles – 28 Sep 2013
- Back to School: Intro/Index – 26 Sep 2013
Advertisement by Google
(sorry, only few pages have ads)

