Child Diseases Parents Should Know – Part 10
When we began this journey through a pediatric resident’s “second brain” of commonly common child diseases, I had no intention on making it such an effort with this many parts; but, then again, I never do.
I’m realizing now that it’s a “no win” effort; because, after all, “how common is common?” The diseases could just keep on coming – but they won’t because I’m ending this effort today.
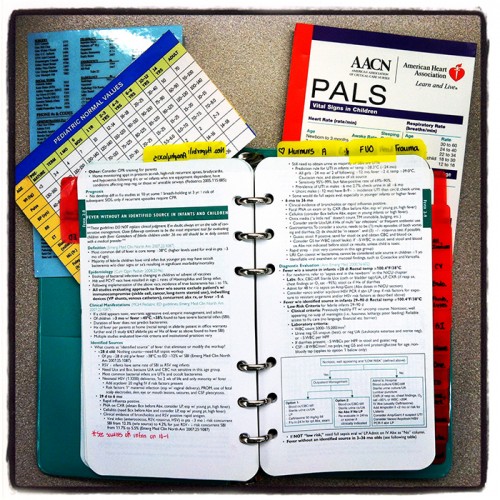
One caveat I forgot to mention before: “Second Brain” notebook kept by all pediatric residentseven though every single one of the pediatric residents in every program around the country have a “second brain” they’ve carried in their coat pocket for all four years of medical school and then through residency, none of them turn out the same.
All of ours were different and we protected them like our kids; because, holy-heaven-above-forbid, if they were ever lost or stolen we would pretty much need to start the whole six years over again from scratch.
Sort of kidding, I guess; but, I did hear a friends voice crack when they related how they couldn’t find theirs anywhere. You see, it not only becomes a reference source for late night call, but is our “journal” or “personal diary” of six or more years of patients we’ve helped and sometimes lost, marathons without sleep, cases we’ve worked up and presented…
That’s why they’re all unique: our experiences were all unique – and that’s why I could never (except arbitrarily) end this article. So, let’s wrap up with some “fun” diseases (for doctors to talk about – NOT to have).
The Final: “Diseases All Parents Should Know” (for now)
Lyme disease
While I was a pediatric resident on the west coast, I was asked to do a presentation at the American Academy of Pediatric’s (AAP) national meeting in Chicago and chanced to meet a few other residents training on the east coast — and to get a peak at their “second brains.”
That began my fascination with the things because of how fundamentally similar they were to ours on the west coast while still having some glaring differences; one of which was that THEY had entries for Lyme Disease with many check-marks (actual patients) and I had never seen a case at that time. I, on the other hand, had an entry for Rocky Mountain Spotted Fever with a few check-marks and they had none.
 The “target” rash associated with Lyme DiseaseBoth of the diseases are caused from tick bites, both cause rashes, both have substantial symptoms with frequent complications BUT their respective carrier ticks just happen to live in different sides of the continent, or at least in different climates.
The “target” rash associated with Lyme DiseaseBoth of the diseases are caused from tick bites, both cause rashes, both have substantial symptoms with frequent complications BUT their respective carrier ticks just happen to live in different sides of the continent, or at least in different climates.
After the tick bite from an infected tick, Lyme Disease takes one or two weeks until symptoms occur. The problem is that the diagnosis is difficult for SEVERAL REASONS: 1) Not everyone develops the flu-like symptoms of fever, chills and body aches; 2) Not everyone develops a rash; 3) IF a rash develops it has several different shapes; 4) some of those shapes are also caused by other diseases; and, 5) It’s only common in certain localities so infected travelers (those who don’t know how to precaution against tick bites) are being seen by doctors who don’t even think about the disease.
There is a hallmark rash (if it does come) shaped like a “target” which makes the diagnosis substantially easier. Unfortunately, in many if not most cases it’s only the “pattern” made by much laboratory work and the exclusion of other more common diseases which enables making the diagnosis.
Only those ticks who have bitten mice or deer infected with the bacteria Borrelia Burgdorferi cause the Lyme Disease which is treated with courses of antibiotics.
Rocky Mountain Spotted Fever
I must admit that it’s sort of prideful having a disease named after the area you live in; but, the truth is, there is more Rocky Mountain Spotted Fever (RMSF) disease in the southeastern US than anywhere in the Rocky Mountains.
 Boy with rash of Rocky Mountain Spotted FeverSo, the battle between the two tick-born diseases is more a continuation of the North versus South strife than anything East vs. West. That said, the extreme rise in the last nine years from one or two cases per year to over FIFTY per year in 2011 has Arizona government-types scurrying around for explanations.
Boy with rash of Rocky Mountain Spotted FeverSo, the battle between the two tick-born diseases is more a continuation of the North versus South strife than anything East vs. West. That said, the extreme rise in the last nine years from one or two cases per year to over FIFTY per year in 2011 has Arizona government-types scurrying around for explanations.
On the whole, RMSF is much more easily diagnosed and handled than Lyme disease, if you want to call what we go through “easy.” If a tick which has been infected with Rickettsia rickettsii bites a human, usually within one to two weeks they develop a fever to 103 or 104°F, headache, chills, abdominal pain, and diarrhea – in short many of the symptoms of the “flu.”
Five to 10 days after that, the petechial rash develops on their wrists, ankles, palms, soles and forearms; then progresses, especially in children, to other parts of the body. Muscular and joint pains also ensue.
It’s a hard-shelled Dog Tick which carries RMSF as opposed to the Deer Tick for Lyme Disease. Both can be treated with antibiotics and the earlier the better. Often, in endemic areas, a person with “flu” symptoms, who says he was bitten by a flea, gets immediate treatment for RMSF based on presumption, even without a definitive diagnosis having been made.
-
How To Deal With Tick Bites
- ☞ Wear light colored clothing so as to easily spot ticks
- ☞ Spray clothing with repellant containing DEET
- ☞ Any dogs in your party MUST be wearing a flea/tick collar (for several days previous)
- ☞ Check yourself and others every two hours while in the field and more fully and carefully in the tub or shower immediately after the day’s activity
- ☞ Finding a tick, note and record coloration and markings for later ID if you become ill
- ☞ Use tweezers to grasp tick by mouth parts as close to skin as possible
- ☞ Pull gently, straight out of skin. Don’t twist or jerk, because that can cause mouth parts to break off into skin
- ☞ Avoid squeezing or crushing the tick
- ☞ Clean the bite site and hands with rubbing alcohol or soap and water
- ☞ Flush the tick down the toilet, don’t throw a live tick away in the trash can
Seasonal Allergies
 6 year old boy with marks of allergy skin testsAllergy symptoms – sneezing, watery-itchy eyes, stuffy-itchy nose and post nasal drip with cough – which are an affliction to you only in a particular season (notably fall) are known as “Hay Fever.” In the purist sense it’s an allergy to the hay which ripens in that season.
6 year old boy with marks of allergy skin testsAllergy symptoms – sneezing, watery-itchy eyes, stuffy-itchy nose and post nasal drip with cough – which are an affliction to you only in a particular season (notably fall) are known as “Hay Fever.” In the purist sense it’s an allergy to the hay which ripens in that season.
However, as a generality, Hay Fever is only a small part of the larger world of allergy effecting the portion of the population who have inherited the “ability to be allergic” known as: Atopy.
Individuals with that propensity can become sensitive to anything – given enough exposure, in the right amount, for the right length of time. Children are born with Atopy but not with specific allergies to cats (for example). After getting a cat, atopic children will eventually become allergic to cats and develop symptoms – or whatever they are exposed to consistently.
Additionally, the constellation of allergic symptoms for any one person, are specific to that individual. Whereas a mother may have Hay Fever triggered in the fall, a child may have asthma triggered by cats or eczema.
There is nothing that can undo the genetics of Atopy, but there are treatments (including antihistamines, inhalers, allergy shots and steroids) to treat the varied diseases and triggers. Several other articles have already been written on various aspects of Allergy and I’m sure there will be more.
– – 0 – –
Like I said at the beginning, this list was a valiant attempt to publish the commonly common diseases parents should know about; but, like it was destined to do from the start, got out of hand. More could/should be added but for now let’s leave it with the recommendation to use the “search” box at the top to check if anything you want to know has already been written about.
If not, use the “contact” form below to drop a line and ask a question.
11 Posts in Childhood Diseases (childdiseases) Series
- Part 10 - Lyme - Allergies – 9 Oct 2014
- Part 9 - Impetigo - Influenza – 1 Oct 2014
- Part 8 - Polio - MRSA – 23 Sep 2014
- Part 7 - Meningitis - Scarlet Fever – 11 Sep 2014
- Part 6 - Diptheria - Tetanus – 3 Sep 2014
- Part 5 - Varicella - Rubella – 18 Aug 2014
- Part 4 - Rotavirus - Kawasaki's – 10 Aug 2014
- Part 3 - Hand, Foot, Mouth and Fifth disease – 29 Jul 2014
- Part 2 - Otitis, Glue ear – 21 Jul 2014
- Part 1 - Croup, Bronchiolitis – 17 Jul 2014
- Childhood Diseases Parents Should Know: Intro/Index – 15 Jul 2014
Advertisement by Google
(sorry, only few pages have ads)