Cardiac Arrest: Commotio Cordis – Prevention, Return To Play
Astin, the 17-year-old who suffered cardiac arrest when he was hit in the chest by an elbow playing baseball, is back for his 2nd follow-up. Remember, last visit he was depressed with worry over all the junk he had read on the internet and you (well I) assigned him some homework.
For the third article in the series we’ll talk about what we can do to “prevent” Commotio Cordis (CC, his final diagnosis) and help him decide about going back to play baseball in competition.
Higher incidence of Commotio Cordis in Lacrosse
Ok, do you want to take the lead on this? Come on, it would be fun. You’ll probably make a big difference in his life – and might even get a Christmas card.
Alright, I’ve got your back. But don’t say I didn’t try.
Commotio Cordis: Childhood Cardiac Arrest
Prevention and Return to Play
Astin and his dad had tried to understand the near fatal cardiac arrest he had by looking it up on the internet.
They admitted they hadn’t actually seen any page from sources like the CDC, American Cardiology Association or American Pediatric Association but were then more confused than ever wondering if they had been given wrong advice in the hospital.
A new heart murmur that you discovered last visit was probably an “innocent” murmur of childhood so you began allowing him to slowly rehab back into physical activity by walking/jogging an hour each day with his father to slow him down.
What you don’t yet know is that after you left last time, on our way back into the waiting room, his dad cornered me again over his anxiety so I ordered a weeks worth of cardiac monitoring while they began their exercises.
Astin! It’s great to see you so chipper this morning. Is it because you like hearing my jokes or did you finally get a date for the dance?
By the way, how did you like that monitor? … Oh, yea? … You’ve got to be the first person whose ever said that. Nobody ever likes those things. They are a real pain the butt.
However, it did show me… … absolutely nothing. Which is a good thing! Not one single abnormal beat the entire week you wore it, even when you exercised.
EXCEPT, there was that one day when it seemed like you must have exercised twice cause your heart-rate went up – did you wear it while you went to ask for that date?
While you’ve been talking, you’ve been examining his heart and circulatory system which are completely normal. When you had him exercise, it took longer for his heart rate to go up than last time and he recovered more quickly – all back to the normal he was when you did his pre-season physical. You don’t even hear that heart murmur anymore.
You commented on it and asked how the running with his dad had gone the past couple weeks. His dad grinned when Astin replied: “dad’s much improved.”
Yea? What does “improved” mean – that you don’t have to carry him any more?
Listen Astin, it’s great to just be here talking to a kid who almost asked St. Peter for the key-code to the security gates – and I would like to get to know you better; but, I
can tell you your body is absolutely doing great now and I’m wondering how your mind is doing. Did you look up better information on the internet about Commotio Cordis?Not to your surprise but pleasure he had actually done quite a bit of research like you asked and was much more relaxed as you went through all the worries that had plagued him last time.
His “commotio cordis” was NOT the heart “attack” of the internet. It was more of a “freak accident” where survival is much more common than in the other causes of “sudden arrest” seen in young athletes.
Wow! I’m impressed.
Your incident has effected me too. After your newspaper publicity I talked to two friends from medical school who both called me about CC patients they’ve seen. One a high-school Lacrosse player a couple years ago who still has some nervous system problems.
The other a 12-year-old catcher who is still in the hospital (in the next town over). He wants to refer him to me for follow-up when he’s discharged.
We need to move the appointment along and there’s three things we still need to cover: Survivability, Prevention and Return to Play.
Survivability
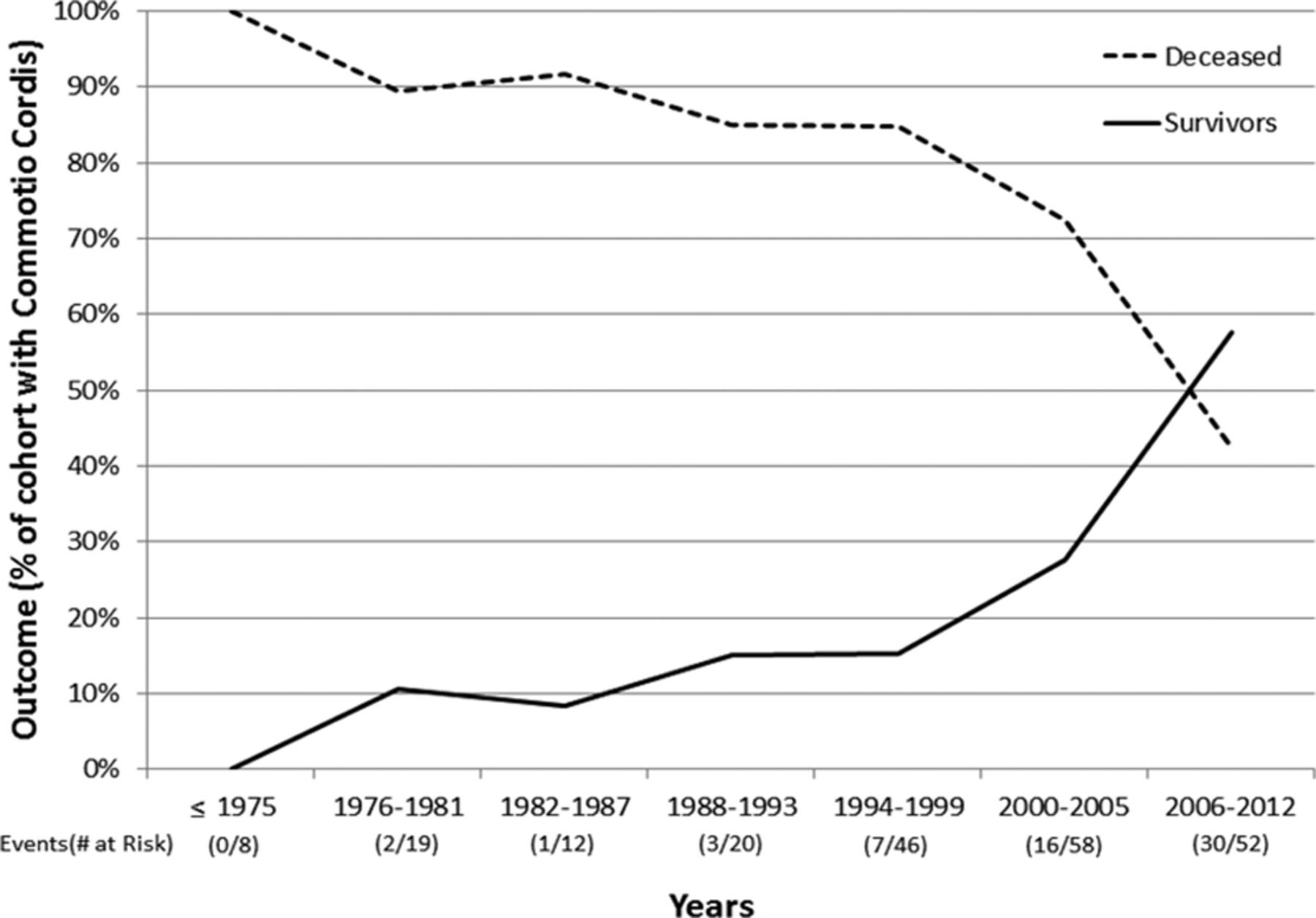
First, we already know that for Commotio Cordis, the old data doesn’t apply any more. Taking all the cases of CC in the database of the US Commotio Cordis Registry (USCCR), only 15% of patients survived.
That figure is for all years and lumps everything together, even those cases where everybody just stood there screaming and flailing, waiting for the ambulance to arrive.
However, we now know that when you separate out cases where CPR was started within 3 minutes, 68% survived; and, if CPR was delayed by more than 3 minutes, that leaves only 3% survivors!
Which means that survivability in Commotio Cordis has steadily increased since 1975 when record-keeping began. Now more kids survive than don’t. Probably due to a much more knowledgeable public and more availability of resuscitation equipment.
Prevention
So far we know a lot of things that don’t help prevent Commotio Cordis; but, only two things that definitely do.
About a third of children who get CC do so in competition while actually wearing a chest protector. So, they don’t seem to help much – at least how they are currently designed.
On the other hand we absolutely know that the “hardness” of the ball definitely does make a difference. All the statistics I’ve already given are for standard baseballs. However, when they tested impacts on pigs, the rates of producing Commotio Cordis with ventricular fibrillation went from 70% to 19% with what is now known as a “safety baseball.”
And we definitely see a correlation between standard and safety baseballs in children when we retrospectively look at our sports statistics.
That’s why we now recommend rule changes to require the use of safety baseballs in competitions for children under 13.
That’s it. That’s all we’ve got. Commotio Cordis is an accident and there are only limited ways to prevent an accident. BUT, that’s only part of the issue.
Just as important is to prevent the RESULTS of an accident – in this case that’s usually death. We’ve discovered that being prepared to recognize and treat the accident on the playing field just may be the single best approach we’ve got!
Coaches and staff who can recognize, treat and use an Automated External Defibrillators (AED) are the single best asset to preventing death from Commotio Cordis in child athletes.
Therefore, another rule must be that an AED should be accessible at any organized sporting event within a minute of the playing venue so that a shock can be given within 3 minutes of an athlete’s collapse.
Coaches and staff should have an action plan and practice it at least yearly. Parents should make sure such plan and training is present where their children play.
Secondary prevention may involve avoidance of certain sports until the age of 18 years or older. After baseball, the most occurrences of commotio cordis per year are in softball, hockey, football, lacrosse and martial arts. But, we must keep in mind that CC is like “lightening striking” and kids are probably more likely to get a concussion from riding bikes.
Return to Play
That’s a lot of talking Astin, but you did want to hear the truth about the stuff you were reading.
Now what do you want to know about returning to play? A couple things that might help would be to know that there is currently (2016) only one known case of CC recurrence!
And, there is also no evidence that survivors of commotio cordis have a greater risk of future arrhythmic events – I’m only talking about your heart rhythm not your dancing.
All of the heart associations have some guidelines and I’ve made you a copy you can show your coaches. To even make the diagnosis I had to first make sure that you did NOT have a hundred or so other possible problems – I even did drug testing on you while you were still goofy and am sure glad you’re making clean choices with your life.
And, we’ve looked at your heart from top to bottom as the guidelines suggest and don’t see any damage or problem from the CC.
So, you’re cleared medically to return to play – if you still think you can have some fun doing it. Just play smart and I’ll see you in two months for another follow-up or you can call anytime if you think of more questions or have anything else pop up. I like to keep watch on you for a year then go back to normal checkups.
Now that wasn’t so bad was it? As patients go Astin was very rewarding – cooperative, interested, easy to work with and a great outcome. I’ll let you know if anything changes and feel free to stop by and see another patient with me any time you’d like.
Safety recommendations for the care and prevention of Commotio Cordis in children
- Measures should be taken to ensure successful resuscitation of commotio cordis victims, including training of coaches, staff, and others to ensure prompt recognition, notification of emergency medical services, and institution of cardiopulmonary resuscitation and defibrillation
- A comprehensive evaluation for underlying cardiac pathology and susceptibility to arrhythmias should be performed in survivors of commotio cordis
- It is reasonable to use age appropriate safety baseballs to reduce the risk of injury and commotio cordis
- Rules governing athletics and coaching techniques to reduce chest blows can be useful to decrease the probability of commotio cordis
- If no underlying cardiac abnormality is identified, then individuals can safely resume training and competition after resuscitation from commotio cordis
[J am coll cardiology 2015 – AHA/ACC SCIENTIFIC STATEMENT]
5 Posts in Child Cardiac Arrest (cardiacarrest) Series
- Commotio Cordis: Prevention and Return to Play – 9 Sep 2016
- Commotio Cordis: Treatment and Prevention – 26 Aug 2016
- Sudden cardiac arrest - case – 7 Aug 2016
- Sudden cardiac death – 26 Jul 2016
- Sudden Cardiac Arrest in a Child: Intro/Index – 25 Jul 2016

