Daily News: Beet Juice & Heart; Telemedicine; Brain Differences & ADHD; Diabetes Cost
Daily medical news, that’s how often it comes across my desk and trying to winnow the fruff while gleaning the critical information for you is a bit time consuming. There are millions of professionals all trying to add their legacy of understanding to the mix of medical care and just one of me.
Sheer amount of even good medical literature is daunting
A good article for you can take me a week or more to write, verify and proofread; and I’m afraid that some news items get the short shriff. There’s only a finite amount of time that I can tolerate sitting here typing.
HOWEVER, let’s just take a stab at presenting a quick synopsis of the articles I actually read TODAY (Thur 6/23/16) – MINUS those that were only skimmed and tossed as obvious self-serving advertisements masquerading as medical articles (over 15 of ’em on Medscape).
Daily News:
Worthwhile, Interesting, Bizarre and Humorous
You do need to understand that me reading the article and evaluating it is one thing; but, reading and then writing about it here with the necessary explanations is quite another so this article may leave some explanations hanging.
OK, [huge breath], let’s tackle this… goin’ in!
Beet Juice and Heart Function – mixed results
Background info: Type II (adult onset) diabetes is really, really bad on blood vessels; some medicines are available to lower blood pressure (BP) when it gets high; Spironolactone lowers BP and also reduces vessel “stiffness”; beet juice (organic nitrate) also reduces vessel stiffness but doesn’t lower BP.
Diabetic and pre-diabetic volunteer patients had a ton of specialized cardiovascular testing done then were randomly assigned to the four treatment groups receiving the matrix of spironolactone vs control and beet juice vs control for 6 months. All the testing was repeated at 12 weeks and 24 weeks.
Results: Spironolactone did “flexible-ize” the heart, the control did not but the heart improvement wasn’t what they expected. The researchers say: “spironolactone’s cardiac changes were highly favorable,” but the blood-vessel findings went against their initial hypothesis. Also, “(it) may be related to the way we measured it… (but) cardiac function doesn’t work so well for people with diabetes on doxazocin (the ‘control’ medicine).”
Beet juice did improve some of the testing more than control but not what they expected or could explain.

Meaningfulness: Perhaps doctors should/could use spironolactone for new uses but this study didn’t show in what way and what difference to expect. Beet juice could-possibly-might be useful; but, again for what and how wasn’t really studied. “More study is needed.”
Quality of Life in Diabetes
Background info: Medicine knows more about controlling diabetes today than we ever have; but, many patients: one – don’t have access to the best medical care; two – have doctors who even practice it; or, three – will follow the lifestyle changes even if their doctor does warn them. Diabetics really have issues with their heart and vessel systems – in addition to problems with nearly every other system.
Results: Over a full 10 year period these guys tried really, Really, REALLY hard to make a financial/health benefit case for a really, Really, REALLY intensive lifestyle intervention program they designed. 5,145 middle-aged, 45-74 year-old, type II diabetics were “treated” (really) to the best possible health care interventions or “normal” education (actually better than most patients get) to see if there was a difference in things like “death,” “heart attack,” “stroke,” or hospitalization for angina. They also measured quality of life stuff like physical and social function and depression.
Unfortunately the study was stopped after 9.6 years due to the futility of measuring the intended outcome of death etc.. There was no difference in those catastrophic effects in the short time they had for the study. BUT, there were differences in the other quality of life stuff; including: they lost more weight and kept it off for many years, AND their new life-styles even helped mitigate (minimize and delay) the normal effects of aging!
Meaningfulness: To my mind this absolutely verifies the good medical care that we all know we SHOULD be providing, and highlights the embarrassment we should feel for not doing it. The program was designed and delivered so well that it would be worth paying for; BUT, it is doubtful that many could afford the intense follow-up and coaching they gave these people. “More study is needed.”
Doctoring Via Telemedicine
I know I said I was going to weed out self-serving advertisements; however, this article intrigued even though I was disgusted that the journal fell for this junk “press release.”
Basically, it gave an example of some employee who felt nauseated, ostensibly had “abdominal pain” and went down into the lobby where she works. She cloistered herself in a Kiosk, and had a “consult” with a “nurse practitioner for $15” – supposedly having an “examination using equipment provided in the Kiosk” – to find that she still ought to go get an ultrasound for a “possible liver problem stemming from an intestinal infection.”
The article exclaimed that the $15 for the nurse visit was “far less expensive than an urgent care visit with a doctor” then went on for a couple pages to proclaim the few employers who were paying $30,000 – $60,000 for Kiosks from a specific company “instead of staffing a full clinic onsite.”
The obvious ad copywriter wildly threw around big medical words for effect stuffed with allusions and no real specific facts. Abdominal pain and nausea could be anything from “stomach flu” to gall bladder to appendicitis to muscle strain and a thousand more. $15 is less than a doctor – NO KIDDING! It’s like buying a peanut and saying it’s less than a lobster – get serious! You think all a person with a true “liver disease” needs is a “peanut”???
Calling a video-camera-look-at-her-face (even with those automatic blood pressure and stethoscope machines) a “physical exam” is a bold-faced lie in the first place; and there is no way the nurse got to actually feel her liver through a machine, which is the organ that she CLAIMS was a “problem” – a simple fact for the author to relate if it had actually been true!
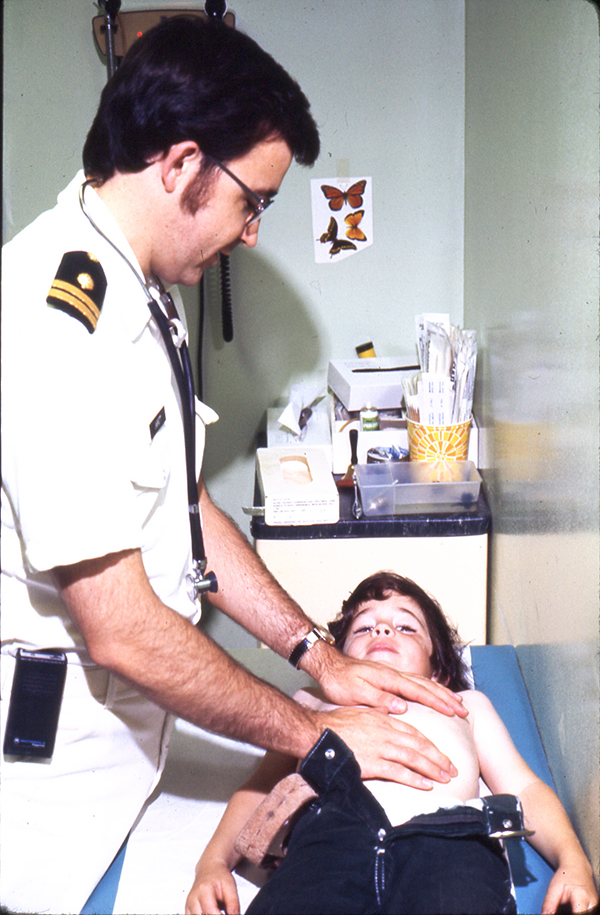
Therefore the hapless patient not only paid $15 for a worthless piece of information, delayed actually seeing someone who would feel her liver, still paid for a possibly (if someone had actually just felt her liver) unnecessary ultrasound and a physician to interpret it – AND STILL NOBODY HAS SPENT THE 30 SECONDS TO ACTUALLY FEEL HER LIVER!
Meaningfulness: While telemedicine Kiosks are here and the practice of medicine is changing this “press release” piece was a clear bunch of clap-trap, written by some marketer that has no clue about what good medicine looks like and the absolutely worst example of telemedicine they could ever pick.
The poor soul’s end statement disclaims: “telemedicine has its limits and they must depend on practitioners to tell patients when they have to see a doctor — in person. We have to rely on their experience and judgment.” Judgement based on WHAT exactly? That they don’t have a clue what they are seeing or doing?
“More study is NOT needed; BUT, this deceptive and disguised advertisement wants you to think it’s cool and go out and buy a Kiosk.” Which is more reprehensible, the author who wrote such a disgusting piece or the – supposed – medical eJournal which printed it as a bonafide article?
Civilian and Military Trauma Plans
The Journal of the American Medical Association published a “commentary” article about the need for better communication and data sharing between the civilian and military medical systems. Their lead sentence: “Since antiquity, with respect to advancing the care of the injured, ‘war has been a very efficient schoolmaster’”, is excruciatingly true.
Their data included the fact that the recent wars had produced the lowest percentage of wounded who died of their injuries in recorded wartime history – 9.3% in Afghanistan and Iraq compared with 23% in Vietnam; and attributed it to three areas of innovative care improvements: bleeding-control, resuscitation techniques and neuro-critical care – innovations that could never be done in centers limited by OSHA and research-oversight committees.
Bottom line: At least 8 emergency/trauma societies and agencies called upon “king obama” to use his pontifical powers to order the creation of a “national trauma care system” (of course with lots more government money) while swearing that “they have no relevant financial interest.” (?) “More action is demanded.”
Outlaw Powdered Alcohol

Background info: Here’s the deal. A guy in Arizona has developed a way to make powdered alcohol and has pushed and connived in every way he knows how to get it approved and sold in the US cause he stands to make HUGE amounts of money; But, state legislatures caught wind and have banded together to pass laws that prohibit the manufacture, importation, distribution and sale of the stuff.
He did submit and have approved his LABEL for the product that looks like children’s “sour powder” then did massive advertising claiming that “it is federally approved.” Still, 32 states have banned powdered alcohol and most others have bills pending. Even Arizona passed the ban but it was vetoed by the governor with the most specious of non-answers to questions.
This stuff has the real potential to become the most inappropriate, difficult to control and deadly temptation to children with absolutely no true socially redeeming value or use. His rebuttal? He name-calls opponents: “unenlightened,” “foolish,” “uninformed” – yea right!
Bottom line: The AMA House of Delegates voted to support federal and state bans of manufacture, importation, distribution and sale of powdered alcohol – lest there should be ANY DOUBT WHATSOEVER whether or not the guy’s claims that it would “help the medical profession” were valid; they are not!
Predicting Cardiovascular Outcomes
Background info: A previous MASSIVE study of heart disease (Framingham) has been the measure of heart disease and directing treatment for several years. The diagnosis: “stable heart disease” has been thought to be a fairly homogeneous group; BUT, in fact MAY have variation in risk up to 1-fold for certain individuals. An Aptamer is a tiny nucleic acid that can bind to certain proteins sort of like an antibody. Researchers in San Francisco at University of California report results of measuring 1,130 different proteins in heart patient’s blood.
Results: They found 9 key proteins that seem to accurately “tattle” on a persons “risk” of adverse events like heart attacks, strokes, heart failure and death better than the Framingham criterion. After these are better validated, they will enable physicians to delineate “very high risk,” “medium risk,” and “very low risk” patients.
Meaningfulness: With such labels, patients may choose to be treated with different regimens and have the motivation to effect difficult life-style changes. These proteins can also now be used to study “lower risk” individuals too. “More research is needed” to define how treatment should be different in each group, otherwise these proteins are merely just “data gathering.”
ADHD, OCD Brain Differences
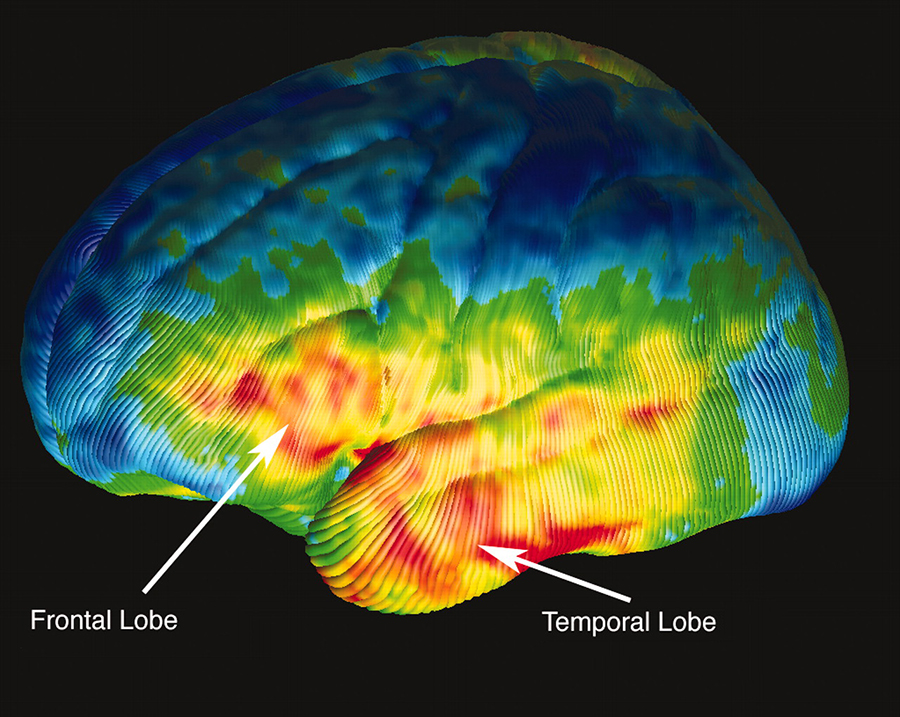
Background info: Stimulant medications are actually the best drug we have in all of psychiatry, producing good benefit in 70% of children with a “diagnosis” of ADHD. Giving them to patients with Obsessive-Compulsive Disorder (OCD) makes them worse. Diagnosis of either condition is based on what observers think of a patient’s behavior – i.e. very difficult at best. Complicated (and expensive) computer and MRI analysis methods have been developed for studying brain structure and functioning (voxel-based morphometry and functional MRI).
Results: Intense computer analysis of combined data from many other large studies (57 studies, 1859 patients and 1533 controls) showed obvious differences in the prefrontal/insula regions. ADHD patients were less functioning and smaller, OCD larger and over functioning.
Meaningfulness: Right now this data is at the stage similar to finding out that apples have red pigment and oranges do not – we knew they were different already – now what? This difference explains why drug treatment is different. Clearly “More research is needed” to now explain what about the 10 – 20% of patients who have BOTH ADHD and OCD symptoms. Are the symptoms only manifestations of and not indicative of the diseases?
Sleep Apnea and Stroke
Background info: Medical school taught us that untreated sleep apnea can cause a whole host of diseases and problems in seeming unrelated organ systems including the heart. Sleep apnea, an aspect of “Sleep Disordered Breathing,” (SDB) is fairly easily diagnosed and increasing in frequency; so is cardiac disease. “Acute Coronary Syndrome” (ACS) = all the heart problems related to angina and heart attacks. “Percutaneous Coronary Intervention” (PCI) = all the “heart cath” procedures related to “fixing” ACS. “Major Adverse Cardiac and Cerebrovascular Events” (MACCE) = the list of “bad things” that happen in the cerebrovascular system: heart attack, stroke, death etc..
Results: In Tokyo patients with SDB (241) were followed prospectively for 5 and a half years trying to validate a measurement of how much apnea patients have with cardiovascular events. The report: “it appears that SDB should be included in treatment considerations of ACS events and primary PCI… to prevent MACCE.” The risk for MACCE based upon age or hypertension is about 1 time greater; but if a patient has SDB they have a 2.5 times greater risk! The study noted that cardiologists rarely even considered the possibility of SDB even though they were performing surgery.
Meaningfulness: The bottom line is: If cardiologists miss the diagnosis of sleep apnea when they do heart-cath interventions on people with MIs and angina, it can come back and bite them in the butt with major long-term crises. Well, actually, it’s the patients who are the ones who suffer and their primary doctors who solve the oversite. They suggest that the cardiologists’ cardiorespiratory monitoring can and should be used to provide a readily available and inexpensive means of detecting SDB (without the mandate for expensive and time-consuming sleep studies).
Childhood Diabetes and Costs
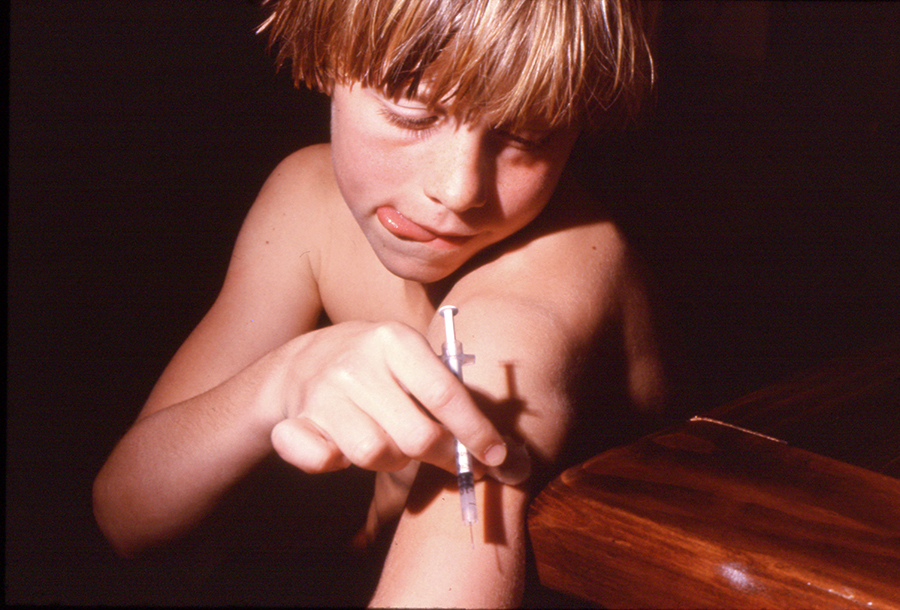
Background info: Childhood diabetes is becoming a significant problem for children, families and insurers. The cost of not only drugs but every aspect of care is out of control due to excessive profit taking.
Results: The article, largely a press release from the company, gave many different statistics. Children under 18 who had insurance, none-the-less spent $2,173 in out-of-pocket costs – five times higher than children without the illness. Children with diabetes visit the ER 2.5 times more often than children without it. Hospital care was used 5 times more often. In all, a year’s worth of care cost them $17,380 out-of-pocket.
Meaningfulness: The excessive profit taking of drug companies and medical material suppliers, coupled with the increasing inaccessibility of primary and specialist physicians, puts families with children who have any chronic problem at real jeopardy – to me a situation for which our industry should be ashamed! And, as disease numbers increase, it means that even more children are subjected to the mercinary effects.
Zika Global Threat
I’ve covered this topic extensively already and I’m about “Zika-ed” out; but, a couple of extra quotes from the meeting could be added.
Background info:
“Mosquitoes are the most dangerous animal… They cause more transmission of disease and more morbidity and mortality than any other animal in the world.”
“Something has happened (mutation) to make this virus what we call neurotropic and to provoke immunological reactions later in adults.”
“In most cases those who contract a Zika infection are not aware they have it. An estimated 80% of people are asymptomatic, and those who do have symptoms are usually mild and include such things as conjunctivitis, a rash, neuralgia, myalgia, and fever.”
Results:
“The World Health Organization (WHO) has declared Zika a public health emergency of international concern.”
Meaningfulness:
We’re in for a bumpy ride on this one folks.