10 Travel Diseases to Consider – Part 2
We’re talking about ‘travel diseases’ which should be considered before taking a trip ‘abroad’ either with or without the family in tow. Yes, from the standpoint of living in the U.S. most of these seem vague and ‘out there somewhere’ but not associated with our daily worries.
Multigenerational family vacation
Unfortunately, they are all too worrisome to nearly everyone else, who all too frequently have a much more accurate up-close-and-personal perspective on them. One which we need to understand if we don’t want to have one of those vacations which ‘keeps on giving’ for a long time.
Travel Diseases To Consider
Before we ran out of paper in the last article, we already mentioned five of the ten major diseases travelers need to be concerned about – Ebola, MERS, CHIKV, Measles and Polio. Despite being quite rare in the U.S., all of them occur in such large numbers around the world, are so contagious to travelers and have such little specific treatment that precautions should be taken.
The remaining five are in the same category.
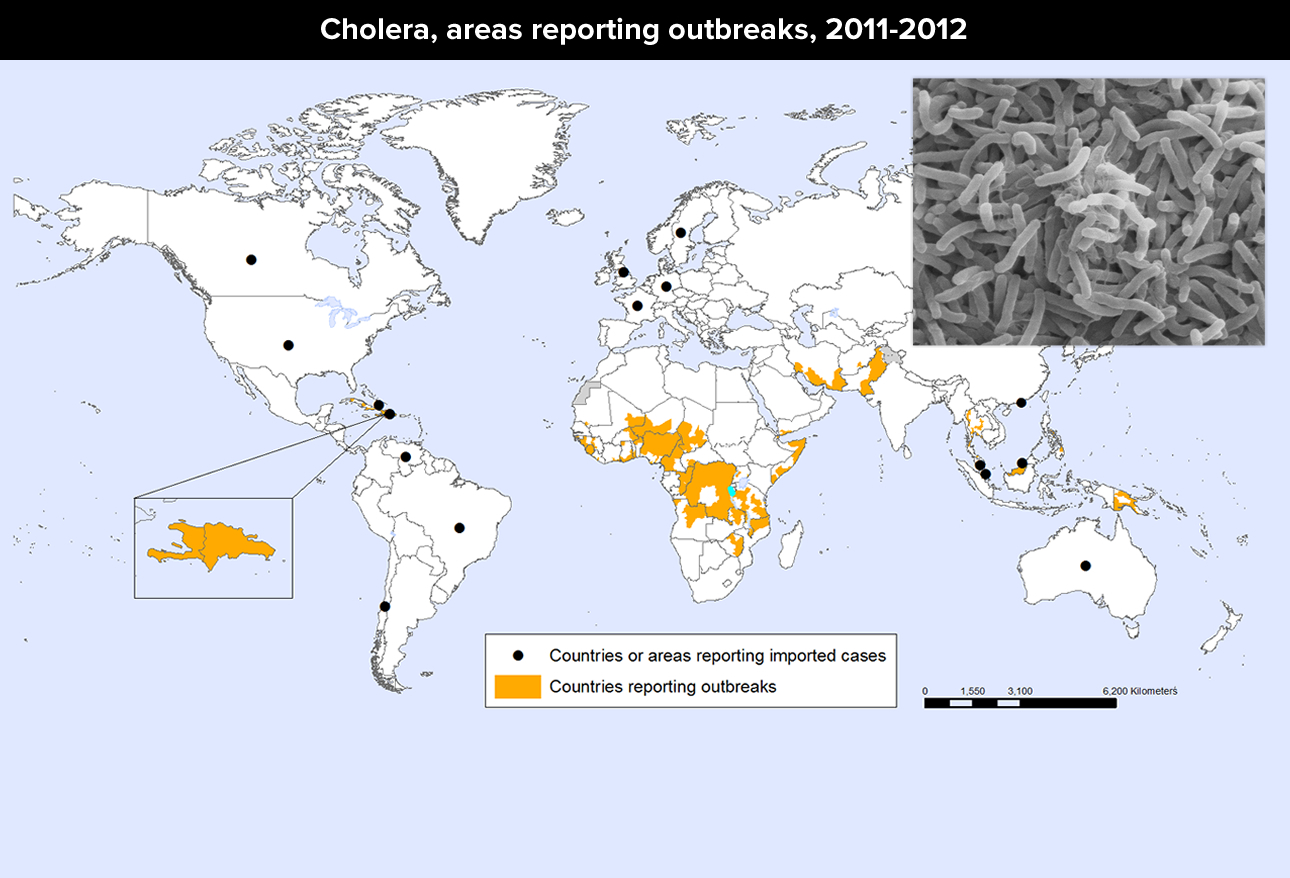
Cholera
Cholera is an intestinal disease in which the bacteria, Vibrio cholerae, produces a toxin that causes intestinal cells to release amazing amounts of water to produce massive diarrhea. It is contracted through contaminated food and water source, largely through inadequate sewage and drinking water treatment – such as in war, famine and crowding.
In up to 10% of cases the disease is so severe and sudden that diarrhea and vomiting can lead to profound hypotension, dehydration, shock, muscle cramps and tachycardia. Death can occur within hours. Rehydration is so critical that the World Health Organization (WHO) has a recommended oral solution to be used in the field even before medical help. Antibiotics may reduce the fluid requirements and shorten the illness. Zinc supplementation may help improve cholera symptoms in children.
Two oral cholera vaccines are available outside of the United States but because each requires two doses, multiple weeks can elapse before those receiving the vaccine are protected. Therefore, vaccination should not replace standard prevention and control measures.
WHAT TO DO: The CDC does not recommend cholera vaccines for most travelers because the available vaccines offer incomplete protection for a relatively short time period. Travelers should always take basic safety and hygiene precautions with food and drinking water, even if they have been vaccinated.
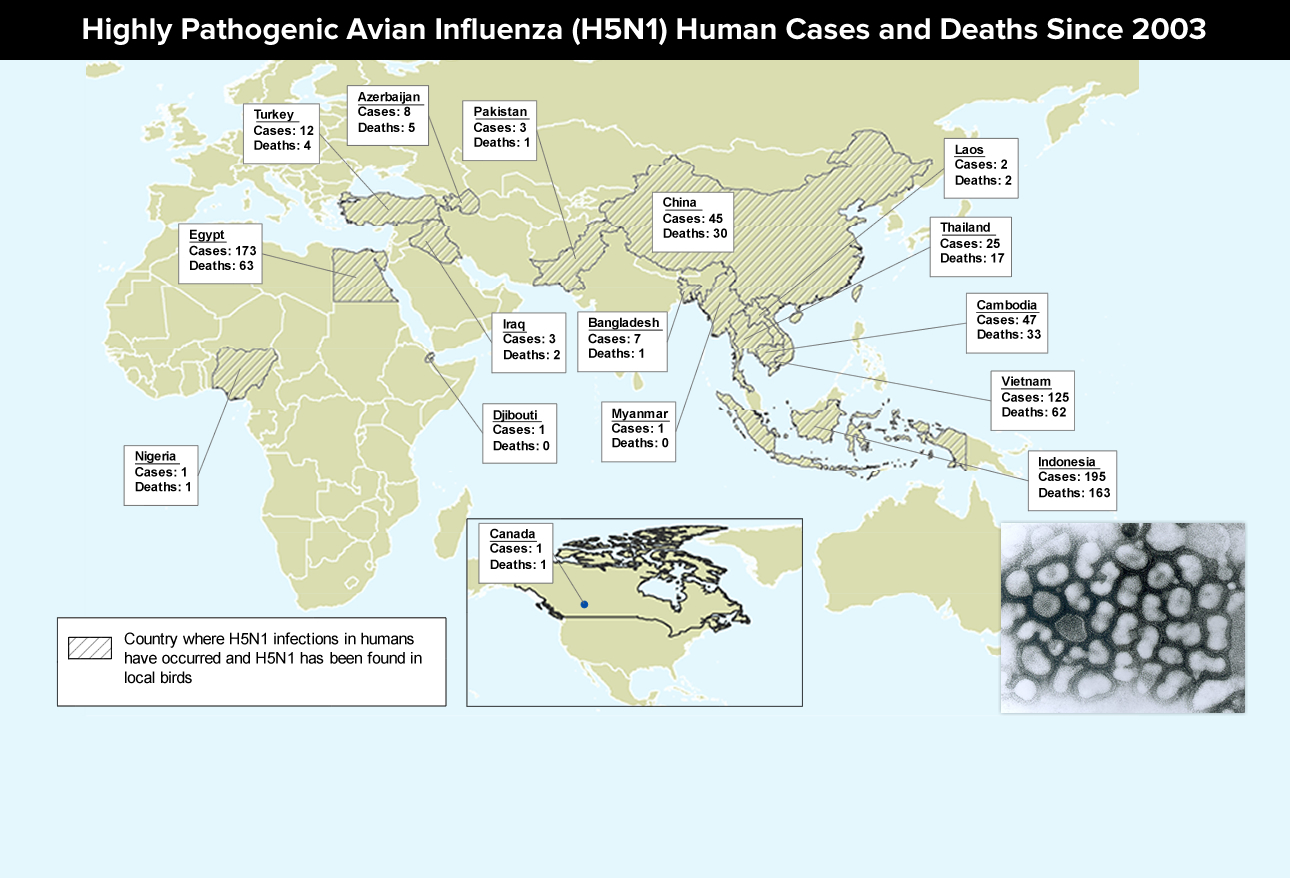
Avian flu
“Flu” or Influenza is a disease that people think they are getting to understand but is becoming more confusing as the years go by because of the “bug’s” infuriating ability to change and modify itself into something new over and over. In addition to the “usual” flu (for which we all get ‘flu’ shots each year) now we’ve got “Highly Pathogenic Avian Influenza (HPAI)” which causes rapid deterioration and kills 60% of those it infects – and there’s at least two types of it! AND, it’s now crossed the ocean to the America’s!
Any influenza infection strong enough to bring a person into the hospital is tested to identify its sub-types; because, it has great implications for not only case outcome but for public health. Low pathogenic infections are generally mild and nonfatal – High Pathogenic, not so much. They often cause multi-organ disease, hypoxemia and secondary infections. The CDC and WHO advise treating type “A” influenza viruses with antiviral medications. The prognosis depends on the type of “A” virus and the disease severity.
WHAT TO DO: The best way to prevent infection with AI A viruses is to avoid sources of exposure. To reduce the risk of exposure to AI and other foodborne diseases when traveling to an area that has an outbreak, avoid visiting live-bird markets, wear protective clothing and special breathing masks when working with birds, and avoid undercooked or uncooked meat. Clinicians treating infected patients should wear appropriate personal protective barriers and follow recommended infection control measures. We note that receiving seasonal influenza vaccination will not prevent infection with AI A viruses, but it can reduce the risk of co-infection with human and AI A viruses.
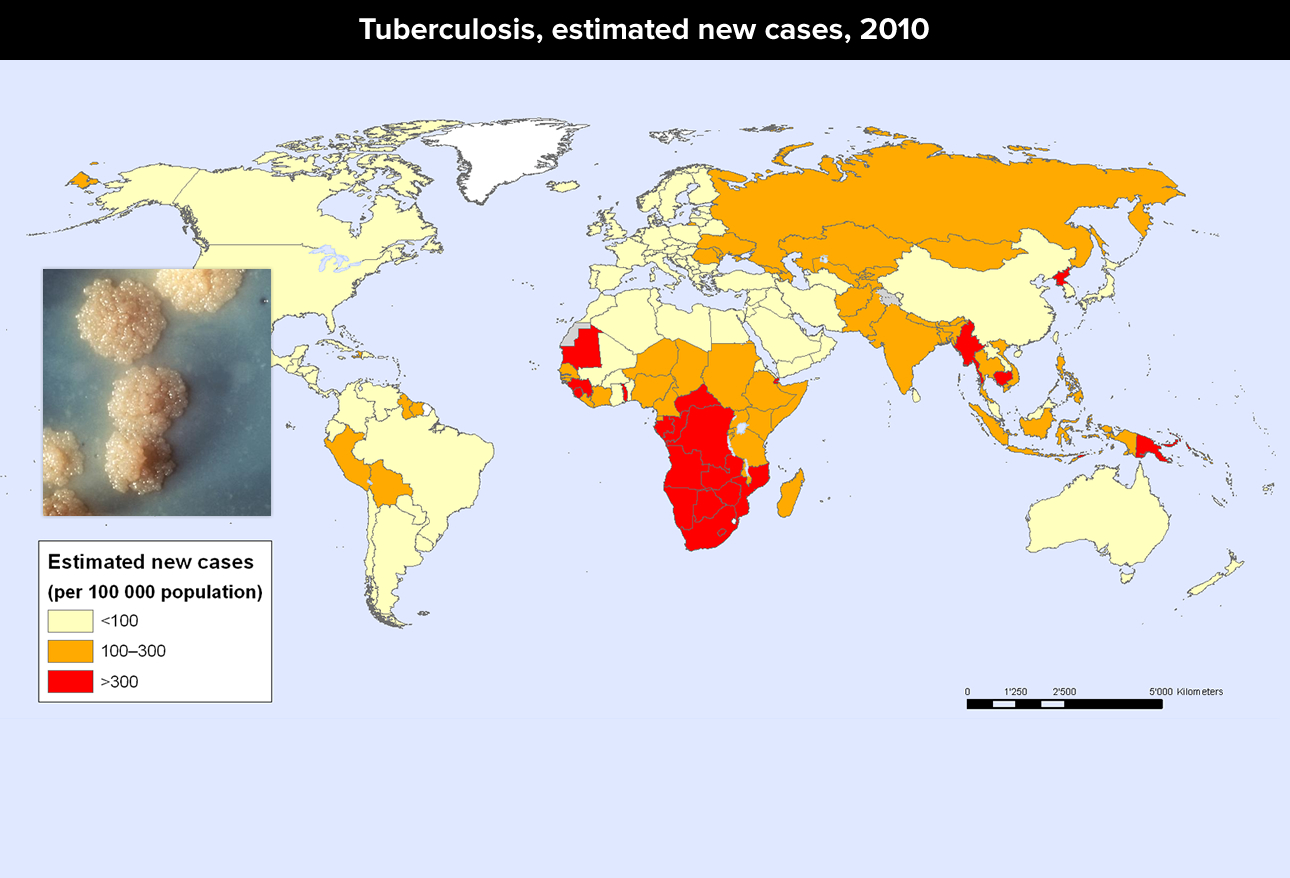
Tuberculosis (TB)
Although Tuberculosis (Tb) was once much worse in the U.S. than it is now, it’s still here. In fact, worldwide, there are 9 million new cases each year and 1.5 million deaths due to the bacteria. It infects the lungs (usually) but also kidney, brain, spine and other organs.
Usually an airborne disease, transmission is by respiratory droplets expelled during coughing, sneezing, speaking, singing and the like. Because it’s so slow growing it can spread before a person really knows the illness they have is Tb. There are tests and in most cases it is treatable and curable; however, TB can be fatal if left untreated. Unfortunately, because it does require a full 6 months of treatment, the cases of inadequately treated disease has resulted in growing rates of drug-resistant disease.
WHAT TO DO: For travelers, standard hygiene precautions should be taken especially within endemic areas of the disease. Those living in such areas may have the bacille Calmette-Guérin (BCG) vaccine is given to infants and children. However, but the vaccine has variable efficacy in preventing adult disease, and BCG can interfere with test results in those with latent disease. An adult who has received BCG may still contract the disease so must be vigilant about giving that information to their doctors.
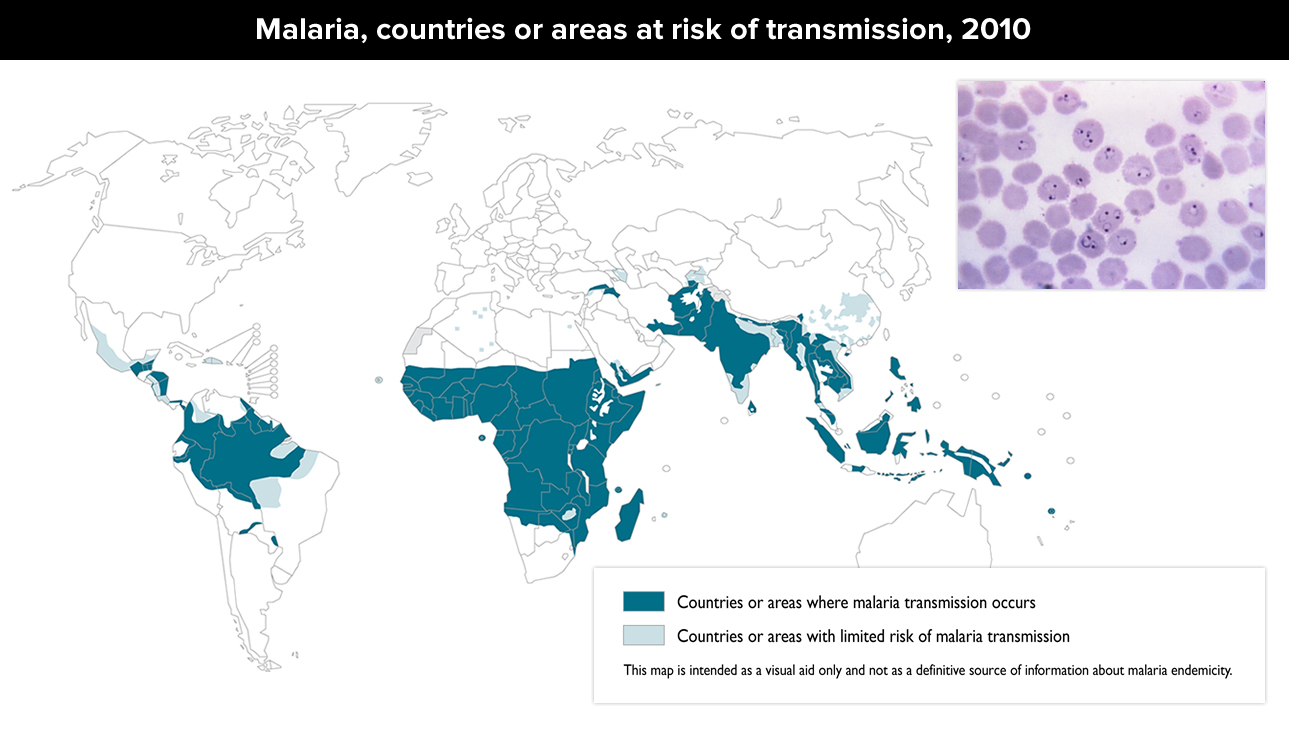
Malaria
Malaria not only takes a bite from a mosquito but a specific type of mosquito. That fact is the only reason we don’t have epidemics of Malaria in the U.S. – we certainly have enough of the beasts! Female Anopheles mosquitoes can get infected with the parasite Plasmodium falciparum which they slather back into humans when they go to get a drink of blood. Oh sometimes it’s blood transfusions, organ transplantation or needle sharing – but mostly it’s mosquitoes.
Humans develop fever/chills, headache, vomiting, muscle aches and anemia about 10-15 days or many months after the bite. The parasite, after multiplying in the human liver, moves on to the blood cells where they break them and cause a recurrence of symptoms. There are drugs to treat (and prevent) the infection; which, of course, the bugs are beginning to become resistant to. Mostly the outcome is good IF it can get diagnosed and treated; however, severe malaria (especially P falciparum) is a medical emergency requiring urgent intervention. Malaria disrupts the blood supply to vital organs and can result in seizures, mental confusion, kidney failure, acute respiratory distress syndrome, coma, and death.
WHAT TO DO: Based on risk travelers should use specific malaria prevention measures (eg, use of protective clothing, insect repellents, insecticide-treated bed nets, antimalarial agents). The particular type of drug depends on the region and the disease severity.
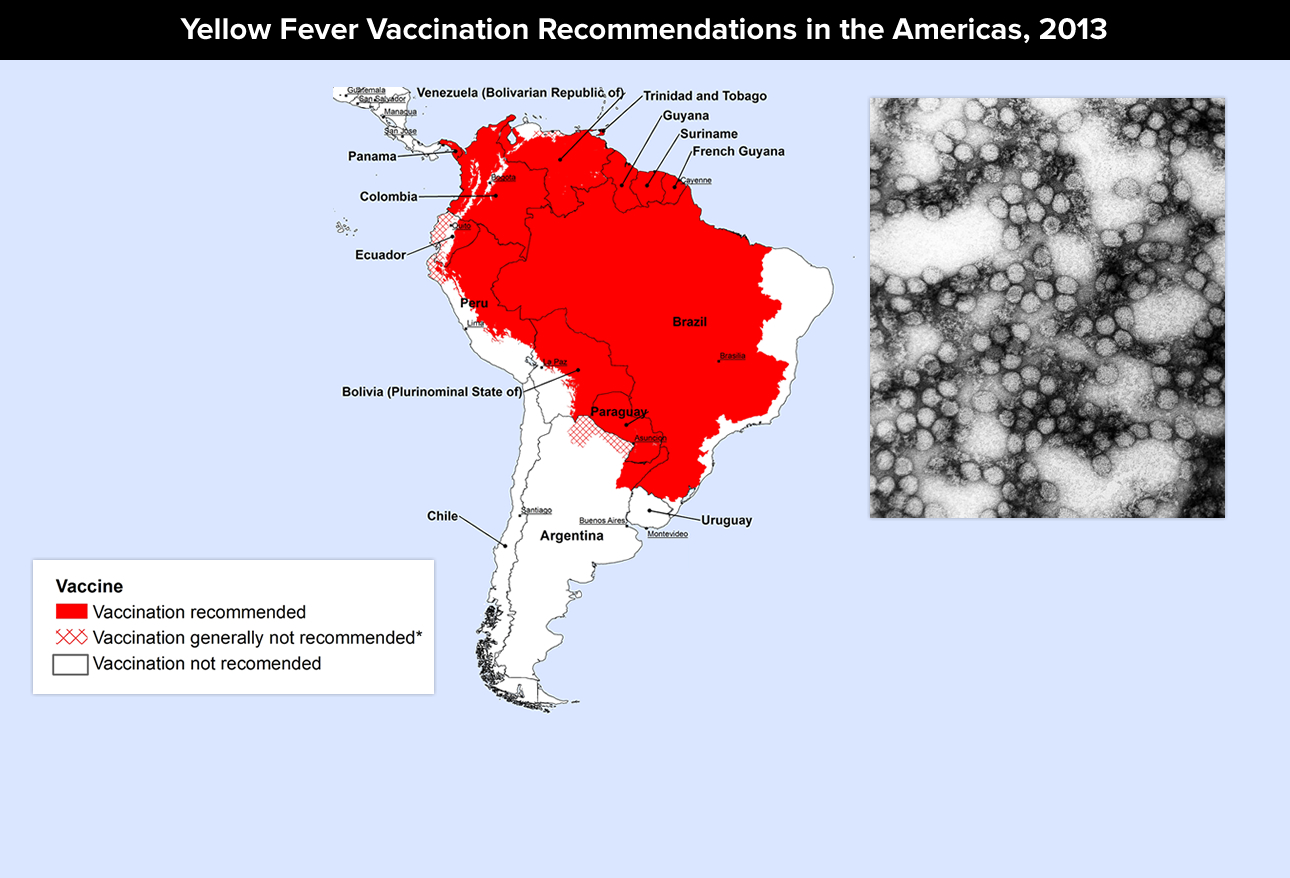
Yellow Fever
Yellow Fever in another one of “them mosquitoes diseases” caused by infected mosquitoes (a Flavivirus). Transmission is between infected primates (human/nonhuman) and has three cycles (jungle, savannah and urban) and three stages (infection, remission and intoxication).
Most develop either no or only mild symptoms initially – sudden fever/chills, severe headache, back pain, myalgias, nausea/vomiting, and fatigue/weakness. Then, after a brief remission of hours to a day, about 15% of patients go on to high fever, jaundice, bleeding, and, eventually, shock with multisystem organ failure, Up to 50% of these patients die within 10-14 days.
It’s difficult to diagnose because it’s confused with other diseases. There are diagnostic tests if the doctor thinks about it; but, there is no specific treatment, only supportive to manage dehydration, respiratory failure, and fever. Unfortunately, such measures are rarely available in poorer regions.
WHAT TO DO: There is a vaccine available that is very effective and which should be taken 10-14 days before travel to endemic areas. Precautions include: sleeping in screened housing, using mosquito repellents (e.g. containing DEET, picaridin, IR3535, or oil of lemon eucalyptus), and wearing clothing that fully covers the body.
Critical To Remember After The Trip
Those are the “big ten” diseases to remember when traveling anytime, not just on vacation. HOWEVER, there are at least three other concepts that are very important.
First, the simple act of merely living in an area confers, over time, a certain “tolerance” to the infections in that area which can make one a bit cavalier to basic and smart health hygiene practices. That “tolerance” does NOT carry with you when you leave the area. You become “fresh meat” to all other infectious agents lying in wait, from travelers diarrhea and colds to those mentioned above.
Second, unless your vacation is fairly long, for the most part you will be coming down with your disease on the way home in the airplane. You will suffer its effects and spread it to others who are just as likely as you to not be immune. Importantly, you will likely seek out medical care from doctors who may have never seen a patient with the disease so will likely not even think of it’s possibility UNLESS YOU TELL THEM WHERE YOU’VE BEEN. Diagnosis might otherwise be delayed until too late to prevent spread or give adequate treatment.
Third, just because your airplane ticket doesn’t state “Africa,” the “Middle East” or some other exotic place, don’t for a minute think you can’t be exposed to one of these diseases. Airports, train stations, hotels, restaurants – in fact any place tourists gather, are prime opportunities of contagion. Remember, all of THEM may be coming back from anywhere with something more than photographs.
Makes you just want to stay home doesn’t it. But, we need to travel so I wrote this article: forewarned is forearmed. (And, I’d really like to see more hand washing and common-sense hygiene being used around me when I’m at restaurants and airports.)
3 Posts in Travel Diseases (10TravelDiseases) Series
- Cholera, Bird Flu, TB, Malaria and Yellow Fever – 11 May 2015
- Ebola, MERS, CHIKV, Measles, Polio – 7 May 2015
- 10 Travel Diseases: Intro/Index – 7 May 2015